Nutritional Assessment

A nutrition assessment is an in-depth evaluation of both objective and subjective data related to an individual's food and nutrient intake, lifestyle, and medical history.
Once the data on an individual is collected and organized, the practitioner can assess and evaluate the nutritional status of that person. The assessment leads to a plan of care, or intervention, designed to help the individual either maintain the assessed status or attain a healthier status.
Elements of the Assessment
The data for a nutritional assessment falls into four categories: anthropometric , biochemical , clinical, and dietary.
Anthropometrics.
Anthropometrics are the objective measurements of body muscle and fat . They are used to compare individuals, to compare growth in the young, and to assess weight loss or gain in the mature individual. Weight and height are the most frequently used anthropometric measurements, and skinfold measurements of several areas of the body are also taken.
As early as 1836, tables had been developed to compare weight and height in order to provide a reference for an individual's health status. The Metropolitan Life Insurance Company revised height and weight tables in 1942, using data from policyholders, to relate weight to disease and mortality. There has been much discussion about the relevance (and appropriateness) of using the individuals who buy life insurance as a basis for "ideal" height and weight. There are also a number of problems with using a table to determine whether an individual is at the right weight—or even what the "ideal
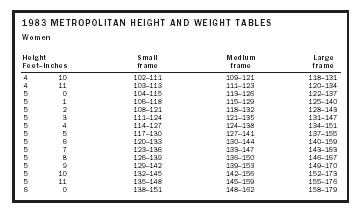
| Women | ||||
| Height Feet–Inches | Small frame | Medium frame | Large frame | |
| 4 | 10 | 102–111 | 109–121 | 118–131 |
| 4 | 11 | 103–113 | 111–123 | 120–134 |
| 5 | 0 | 104–115 | 113–126 | 122–137 |
| 5 | 1 | 106–118 | 115–129 | 125–140 |
| 5 | 2 | 108–121 | 118–132 | 128–143 |
| 5 | 3 | 111–124 | 121–135 | 131–147 |
| 5 | 4 | 114–127 | 124–138 | 134–151 |
| 5 | 5 | 117–130 | 127–141 | 137–155 |
| 5 | 6 | 120–133 | 130–144 | 140–159 |
| 5 | 7 | 123–136 | 133–147 | 143–163 |
| 5 | 8 | 126–139 | 136–150 | 146–167 |
| 5 | 9 | 129–142 | 139–153 | 149–170 |
| 5 | 10 | 132–145 | 142–156 | 152–173 |
| 5 | 11 | 135–148 | 145–159 | 155–176 |
| 6 | 0 | 138–151 | 148–162 | 158–179 |
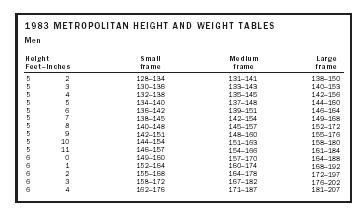
| Men | ||||
| Height Feet–Inches | Small frame | Medium frame | Large frame | |
| 5 | 2 | 128–134 | 131–141 | 138–150 |
| 5 | 3 | 130–136 | 133–143 | 140–153 |
| 5 | 4 | 132–138 | 135–145 | 142–156 |
| 5 | 5 | 134–140 | 137–148 | 144–160 |
| 5 | 6 | 136–142 | 139–151 | 146–164 |
| 5 | 7 | 138–145 | 142–154 | 149–168 |
| 5 | 8 | 140–148 | 145–157 | 152–172 |
| 5 | 9 | 142–151 | 148–160 | 155–176 |
| 5 | 10 | 144–154 | 151–163 | 158–180 |
| 5 | 11 | 146–157 | 154–166 | 161–184 |
| 6 | 0 | 149–160 | 157–170 | 164–188 |
| 6 | 1 | 152–164 | 160–174 | 168–192 |
| 6 | 2 | 155–168 | 164–178 | 172–197 |
| 6 | 3 | 158–172 | 167–182 | 176–202 |
| 6 | 4 | 162–176 | 171–187 | 181–207 |
weight" means. Tables should therefore be used only as a guide, and other measurements should be included in the data collection and evaluation.
In 1959, research indicated that the lowest mortality rates were associated with below-average weight, and the phrase "desirable weight" replaced "ideal weight" in the title of the height and weight table.
To further characterize an individual's height and weight, tables also include body-frame size, which can be estimated in many ways. An easy way is to wrap the thumb and forefinger of the nondominant hand around the wrist of the dominant hand. If the thumb and forefinger meet, the frame is medium; if the fingers do not meet, the frame is large; and if they overlap, the frame is small.
Determining frame size is an attempt at attributing weight to specific body compartments. Frame size identifies an individual relative to the bone size, but does not differentiate muscle mass from body fat. Because it is the muscle mass that is metabolically active and the body fat that is associated with disease states, Body Mass Index (BMI) is used to estimate the body-fat mass. BMI is derived from an equation using weight and height.
To estimate body fat, skinfold measurements can be made using skin-fold calipers. Most frequently, tricep and subscapular (shoulder blade) skin-folds are measured. Measurements can then be compared to reference data—and to previous measurements of the individual, if available. Accurate measuring takes practice, and comparison measurements are most reliable if done by the same technician each time.
To estimate desirable body weight for amputees, and for paraplegics and quadriplegics, equations have been developed from cadaver studies, estimating desirable body weight, as well as calorie and protein needs. Calorie needs are determined by the height, weight, and age of an individual, which determine an estimate of daily needs.
The Harris-Benedict equation is frequently used, but there are quicker methods to estimate needs using just height and weight. Opinions and methods vary on how to estimate calorie needs for the obese . As previously mentioned, body fat is less metabolically active and requires fewer calories for support than muscle mass. If an individual's current body weight is more than 125 percent of the desirable weight for the individual's height and age, then using body weight to estimate calories needs usually leads to an over-estimation of those needs.
Biochemical data.
Laboratory tests based on blood and urine can be important indicators of nutritional status, but they are influenced by nonnutritional factors as well. Lab results can be altered by medications, hydration status, and disease states or other metabolic processes, such as stress . As with the other areas of nutrition assessment, biochemical data need to be viewed as a part of the whole.
Clinical data.
Clinical data provides information about the individual's medical history, including acute and chronic illness and diagnostic procedures, therapies, or treatments that may increase nutrient needs or induce malabsorption . Current medications need to be documented, and both prescription drugs and over-the-counter drugs, such as laxatives or analgesics, must be included in the analysis. Vitamins , minerals , and herbal preparations also need to be reviewed. Physical signs of malnutrition can be documented during the nutrition interview and are an important part of the assessment process.
Dietary data.
There are many ways to document dietary intake. The accuracy of the data is frequently challenged, however, since both questioning and observing can impact the actual intake. During a nutrition interview the practitioner may ask what the individual ate during the previous twenty-four hours, beginning with the last item eaten prior to the interview. Practitioners can train individuals on completing a food diary, and they can request that the record be kept for either three days or one week. Documentation should include portion sizes and how the food was prepared. Brand names or the restaurant where the food was eaten can assist in assessing the details of the intake. Estimating portion sizes is difficult, and requesting that every food be measured or weighed is time-consuming and can be impractical. Food models and photographs of foods are therefore used to assist in recalling the portion size of the food. In a metabolic study, where accuracy in the quantity of what was eaten is imperative, the researcher may ask the individual to prepare double portions of everything that is eaten—one portion to be eaten, one portion to be saved (under refrigeration, if needed) so the researcher can weigh or measure the quantity and document the method of preparation.
Food frequency questionnaires are used to gather information on how often a specific food, or category of food is eaten. The Food Guide Pyramid suggests portion sizes and the number of servings from each food group to be consumed on a daily basis, and can also be used as a reference to evaluate dietary intake.
During the nutrition interview, data collection will include questions about the individual's lifestyle—including the number of meals eaten daily, where they are eaten, and who prepared the meals. Information about allergies , food intolerances, and food avoidances, as well as caffeine and alcohol use, should be collected. Exercise frequency and occupation help to identify the need for increased calories. Asking about the economics of the individual or family, and about the use and type of kitchen equipment, can assist in the development of a plan of care. Dental and oral health also impact the nutritional assessment, as well as information about gastrointestinal health, such as problems with constipation , gas or diarrhea, vomiting, or frequent heartburn.
Evaluation
After data are collected, the practitioner uses past experience as well as reference standards to assimilate the information into an assessment that provides an understanding of the individual's nutritional status. The practitioner uses the anthropometric data to assess ideal and desirable weight, as well as skinfold measurements to determine body fat. Height, weight, and age are plugged into the Harris-Benedict equation to determine calorie and protein needs. Using the clinical, biochemical, and dietary data, influences on the nutritional status can be determined. A nutritional intervention, which usually includes dietary guidance and exercise recommendations, is then formulated and discussed with the individual.
SEE ALSO Adolescent Nutrition ; Adult Nutrition ; Anthropometric Measurements ; Body Mass Index ; Dietary Assessment ; Eating Habits ; Food Guide Pyramid ; Nutrition ; Nutrition Education ; Obesity .
Carole S. Mackey
Bibliography
Christie, Catherine, and Mitchell, Susan, eds. (2000). Handbook of Medical Nutrition Therapy: The Florida Diet Manual. Lighthouse Point, FL: Florida Dietetic Association.
Grant, Anne, and DeHoog, Susan (1999). Nutrition Assessment and Support, 5th edition. Seattle, WA: Grant and DeHoog.
Williams, Sue Rodwell (1997). Nutrition and Diet Therapy, 8th edition. St. Louis, MO: Mosby.
Winkler, Marion Feitelson, and Lysen, Lucinda (1993). Suggested Guidelines for Nutrition and Metabolic Management of Adult Patients Receiving Nutrition Support. Chicago, IL: American Dietetic Association.

The other information will be supplied by the VA.