Physicians and Diagnostic Procedures - Other diagnostic tests
If a definite diagnosis cannot be made on the basis of the medical history, preliminary physical exam, and routine diagnostic tests, more specialized tests may be required. What follows is a description, grouped by body system, of some of the other diagnostic tests.
Tests for Mental Disorders
When a physician suspects that a patient has a mental disorder, the physician must first rule out the possibility that the symptoms are caused by a physical illness. After physical disorders have been ruled out, mental-status tests may be administered. These include the Rorschach inkblot test, the Thematic Apperception Test, the Minnesota Multiphasic Personality Inventory, and the Wechsler Adult Intelligence Scale. These tests are used to diagnose various psychological and psychiatric disorders, including depression, paranoia, anxiety, psychopathy, and schizophrenia.
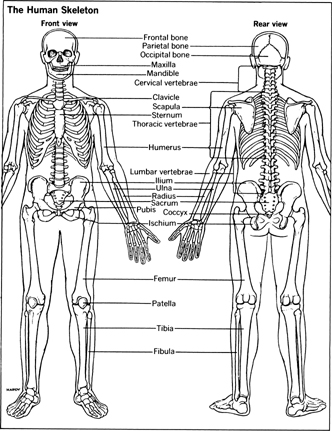
The Skeletal System
The skeletal system includes the bones and cartilage, and the specialist who handles problems of the skeletal system is the orthopedic surgeon. Disorders of the nervous system and joints often overlap skeletal problems and may necessitate tests by a neurologist or rheumatologist.
X rays are the most important diagnostic tool for special investigations of the bones. They can reveal a hairline fracture of a major bone, a bony deposit, or abnormal alignment.
Synovial aspiration , or a synovial fluid exam , involves the withdrawal of a tiny amount of synovial fluid with a needle inserted into a joint. The laboratory analysis of the fluid can help diagnose such problems as gout and some forms of arthritis.
MRI , or magnetic resonance imaging , is a way of creating an image of a body part by taking advantage of the way protons behave in a magnetic field when exposed to a radio-frequency pulse: the way they line up and the form of the radiowave that they emit produces the image. The patient lies down on a table, and a surface coil is applied. The surface coil is the device that emits the radio-frequency pulse. The patient's heartbeat and respiration are monitored, usually by a small band placed around a finger. Next, the table moves the patient so that the area to be examined is inside the magnet. The magnet is in the form of a tunnel and may make some people feel claustrophobic. At this point the noise level increases and may be uncomfortable. Several images are taken, with the table moving slightly between each. MRI is safer than X rays because there is no exposure to ionizing radiation; however, pregnant women and people with implanted stimulatory devices, such as pacemakers, should not have MRI performed.
Nuclear imaging involves the injection, swallowing, instillation, or inhalation of a radioactive isotope (a marker, or tracer) of a substance that is naturally absorbed by the organ or tissues that need observation. A camera sensitive to the radiation emitted by the isotope is then used to create an image that shows the location of the material within the body. Two uses of this technique for skeletal exams are the bone scan and the bone density test. These tests are more sensitive than X rays and can often identify a problem months before it shows up on the X ray. They are used when the X ray comes back normal, but symptoms persist.
In the bone scan the patient receives an injection of an isotope that is taken up by bone tissues. Scanning begins two to four hours later. Either the entire body or just the part under observation is imaged. Injuries, infections, and tumors can all be located with this technique.
The bone density test is used to diagnose osteoporosis, the decrease in bone density that is the major cause of fractures in the elderly. The most accurate bone-density test is dual-energy X-ray absorptiometry (DXA), which uses low doses of radiation— less than is used in an X ray—to measure bone density. The test is painless and safe and can be performed in 5 to 15 minutes.
Ultrasonography is most often employed in skeletal exams to determine whether a “lump” or “bump” is solid or fluid-filled. Ultrasonography follows the same principle that applies to sonar: Sound waves emitted by a transducer are directed at a particular part of the body; they bounce back and are translated into an image. Tissues, bones, water, air—all vary consistently in the way they reflect the sound wave, thus making possible the interpretation of the reflected image.
Arthroscopy is a way of seeing inside the body by using an arthroscope, an optical instrument equipped with lenses and lights that is inserted in a small opening. The area most often studied by this method is the knee.
The Muscles and Joints
The human body has more than 600 muscles of various sizes and shapes, all of them attached to the skeletal system. They enable us to move as they contract. The joints are the spaces between two coupled bones that allow the bones to move in more than one direction. Muscles and joints are the domain of the rheumatologist.
The synovial fluid exam, X rays, MRI, nuclear imaging, and ultrasonography described under the skeletal system are used to examine the muscles and joints as well. When there is a problem with muscle control, inability to relax a muscle, or weakness in commonly used muscles, another test that may be ordered is the electromyogram . This test measures a muscle's electrical potential, which should be zero if the muscle is relaxed. An electrode is attached to the skin over the target muscle and another electrode, in the form of a small needle, is inserted in the muscle. Lead wires from the two electrodes are attached to a monitor, and measurements of the muscle's electrical activity are made while the patient contracts and relaxes it. This test helps determine whether the problem is with the muscle itself or with the nerves controlling it (in which case an electroneurogram is in order).
Joints are prone to stiffness and damage from swelling of the surrounding bursa and tendons. X rays and MRIs will detect damage to the bursa and tendons.
Skin
The dermatologist specializes in treating skin disorders. Many problems specific to the skin can be diagnosed by physical examination and questioning of the patient.
Skin tests are commonly done on allergy sufferers to determine what they are allergic to. In a prick test the forearm is cleansed and a drop each of up to 35 different solutions is placed in rows on the arm. The doctor then takes a small needlelike object and pricks the center of each drop. After 15 minutes any of the solutions to which the patient is allergic will produce a slight swelling much like a mosquito bite. A scratch test is similar; a small scratch is made on the arm and the drop is applied. In the intradermal test the solution is injected. A patch test is done when the patient has a rash, probably caused by something that touches the skin. Patches of possible allergens are placed on the back, and the patient returns in two days for a reading.
Sores that refuse to heal; changes in the shape, color, and texture of warts or moles; and blemishes that bleed or itch are all considered symptoms of skin cancer and should be checked by your doctor. These skin eruptions are usually removed entirely and a biopsy is performed on the tissue. They can be cut out (excised) or removed with an electric needle or laser.
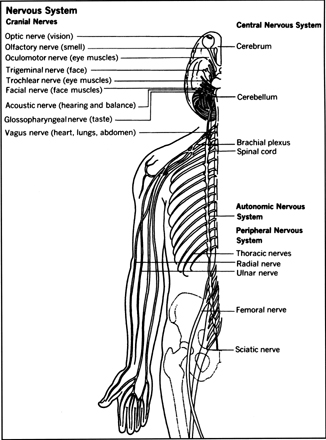
The Nervous System
The brain, spinal cord, and network of nerves make up the nervous system. The neurosurgeon and the neurologist are the specialists.
In a spinal tap , or spinal fluid exam , the doctor inserts a needle into the lower back and removes a small amount of spinal fluid, which is then examined in the lab. The test may cause severe headaches; it is used to diagnose infections, brain hemorrhages, tumors, polio, meningitis, and other conditions. Myelography is a similar study, much more painful, in which a small amount of spinal fluid is removed, dye injected in its place, and X rays are taken while the patient lies on a table. Slipped disks, some types of arthritis, and different types of tumors are commonly diagnosed this way, although the use of MRI (see skeletal system) and computerized axial tomography (CT) are also used and are often done first.
The CT exam is a noninvasive procedure that produces a series of X-ray images showing “slices” of the targeted body part. For the exam, the patient lies on a table (called a gantry) which is then moved into the machine. Several exposures are taken, with the table moving slightly between each. For some studies it is necessary to inject a special dye, which can cause mild discomfort. Some people experience a claustrophobic reaction while inside the machine. CT is about 100 times more sensitive than conventional X rays and is used to detect calcium deposits, tumors, cysts, and abscesses. Because of its sensitivity to tissue density, it can sometimes distinguish benign from malignant tumors.
The brain scan continues to be an important diagnostic tool. This radioisotope study of the brain is used to detect tumors, hemorrhage, stroke, or blood vessel abnormalities.
The brain scan involves the injection in the arm of a radioactive isotope and the scanning of the brain by either a single-photon emission computed tomography camera (SPECT) or a positron emission tomography camera (PET). The SPECT scanner uses gamma rays to create images and the PET scanner uses positrons (a type of subatomic particle found in the nucleus of an atom) to create images. The PET scan is able to read through different depths of tissue, so problems deeply buried in the brain can be detected without surgery.
When the blood supply to the brain is limited by the blocking of the carotid arteries (a condition known as transient ischemic attack, or TIA), momentary loss of brain function can occur and can eventually lead to a stroke. Thus examining the carotid arteries is important if the patient has symptoms or significant risk factors. This can be done by X ray or by ultrasound. In the ultrasound test two techniques are generally used. The first creates images (called duplex) and the second measures the rate and quality of blood flow (called Doppler). Both involve the gentle movement of the transducer slowly over each side of the neck. The procedure takes about 30 minutes.
Patients who have experienced TIA, stroke, or vertigo may undergo ocular plethysmography (OPG) to detect narrowing of the ophthalmic artery. The patient is seated in a chair with a headrest, blood pressure is taken in each arm, and EKG leads are placed on the chest. Anesthetic drops are placed in each eye. The technologist then places tiny plastic cups into the corner of each eye. The cups are attached to wire leads connected to the machine. The patient is instructed to keep the eyes wide open. The machine then produces a slight suction on each eye and measures its pressure.
When epilepsy is suspected, following certain head injuries, or when the patient is experiencing confusion, sleep problems, and even impotence, an electroencephalograph (EEG) may be ordered. The patient sits in a chair while a technologist attaches 16 to 22 electrodes to his or her head. EKG leads are also placed on the chest. The patient then lies down and may even fall asleep. The technologist may instruct the patient to open and close both eyes while a strobe light flashes. The test takes about two hours.
The electromyogram was discussed under the section on muscles. If the muscle is not the problem, the nerves connected to it may be and a nerve conduction study , or electroneurogram , is ordered. This test measures the speed of the electrical impulse across a nerve and the speed of the muscle's response to it. Electrodes are affixed to the skin over the target muscle. The target nerve is then given a mild electric shock. The electrode over the muscle measures both the time between the shock and the response (the muscle will twitch) and the intensity of the response. The corresponding nonaffected muscles are also tested for comparison. There is no hazard, and the shock feels like a mild sting or burn.
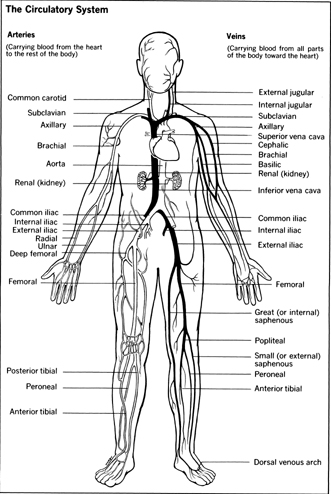
The Circulatory System
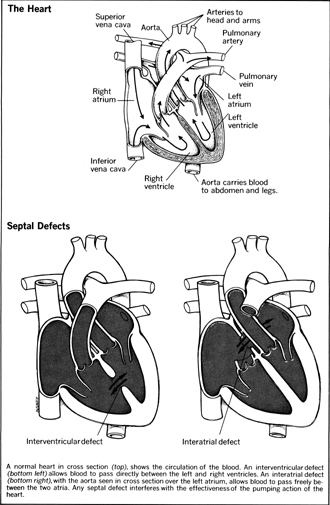
The cardiologist specializes in diseases of the heart and circulatory system. Coronary artery disease is the most common form of heart disease and involves the blocking of the arteries to the heart. There can also be problems with the heart muscle itself, problems with the heart valves, or congenital problems resulting from birth defects.
The electrocardiogram and the stress test have already been discussed. Nuclear imaging, ultrasound, and X rays are also used to detect coronary artery disease. In order to detect exactly how blocked the arteries are and determine the necessary correctional procedure, an angiograph , or angiogram , is done.
The angiograph begins with the insertion of a special needle in a major artery (usually in the groin). A sudden spurt of blood indicates correct positioning. A wire is then inserted through the needle, which stops the bleeding. The wire is advanced to the target area, and the needle is removed. A catheter is then slid over the wire and is advanced to the target area. The wire is then withdrawn. The next step is the injection of a special dye to the target area. To prevent its being diluted it must be injected at high velocity and in large quantity. For most people the injection is extremely uncomfortable, with some reporting severe pain, a feeling of heat, headache, chest pain, or dizziness. The next step involves the rapid imaging of the target area, usually by a series of X-ray pictures. Often different views are needed of the targeted area, which means that the catheter must be repositioned and the dye reinjected. Once the pictures are finished the catheter is slowly removed and pressure is applied to the hole to seal the artery. The pressure involved is intense and lasts for 10 to 15 minutes. Because it is necessary for the patient to be conscious during the procedure, the entire process may cause extreme anxiety, which in turn increases the risk of heart attack. The patient is normally given a sedative to help relieve the anxiety. An overnight stay in the hospital following the procedure is routine. Venography is a similar study of the veins.
Not all people who experience sudden and severe chest pain are having a heart attack. A technique called infarct detection can confirm the diagnosis of heart attack. Normally performed within the first 12 to 24 hours after the onset of the pain, the test involves the injection of an isotope (thallium-201) into a vein. The patient is then positioned under a gamma-ray camera and an image is created of the heart that will make evident any occluded (blocked) vessels. A similar nuclear imaging process is used to obtain information about the heart's wall motion (how well the muscle relaxes and contracts) and ejection fraction (how much blood leaves a chamber of the heart when it contracts). Both tests give valuable information about the heart's health.
While X rays provide more detail, nuclear imaging can also be used to check circulatory integrity , or how open the veins and arteries are. Again, a radioactive isotope is injected into a vein near the target area and images are produced via a gamma-ray camera.
Evaluation of the ejection fraction, valve function, and pericardial fluid (found in the pericardial membrane that surrounds the heart) can also be done with ultrasound. In a process similar to that described earlier for the carotid arteries, echocardiography produces an image of the working heart.
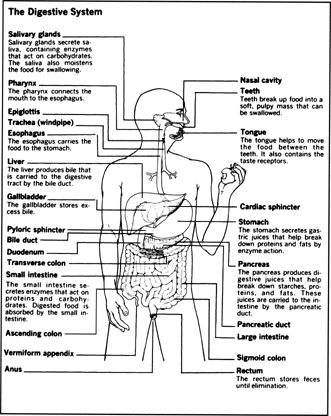
The Digestive System, the Liver, and the Pancreas
The gastroenterologist specializes in disorders of the digestive system and the liver.
As in many other systems, X rays are the traditional diagnostic tool for gastrointestinal problems. Nuclear imaging, however, may be used for some specific complaints. For example, if you're having trouble with heartburn an esophageal reflux test may be done to determine whether or not you have a hiatus hernia. The patient eats nothing the night before the exam. A small balloon is placed over the stomach, held in place by a special inflatable belt. The patient then stands in front of a gamma-ray camera and drinks a glass of orange juice to which a radioactive isotope has been added. Pictures are taken as the fluid moves to the stomach. The patient then lies down on a table and the cuff is inflated, causing the balloon to apply pressure to the stomach. Pictures are taken to see if this pressure causes the liquid in the stomach to back up into the esophagus. If it does, a hiatus hernia is the diagnosis.
In a gastrointestinal examination, X rays are usually taken first, and an endoscopy is done if a tissue sample is needed for biopsy. Endoscopy gives the physician a direct view of the gastrointestinal tract. The endoscope is a flexible tube with a light source, a camera, and instruments for taking tissue samples. The patient eats nothing the night before the exam. After undressing and putting on a gown, the patient lies down and drinks a bitter-tasting local anesthetic to inhibit the gag reflex. A mild sedative is also administered.
The patient lies on his left side with the mouth open. The endoscope is then put in the mouth and advanced down toward the stomach. Photographs are commonly taken, and samples of tissue or gastric juice may also be taken. The exam takes about 2 to 3 hours.
An upper GI may be in order if your doctor suspects an ulcer or tumor. No food is allowed for 8 hours before the test. An injection of glucagon (which may cause nausea or dizziness) is normally given to slow down the movements of the stomach. Next, the patient swallows a small cupful of granular material which produces gas and causes the stomach to distend. Finally, the patient is given a glass of barium and stands with his back to the X-ray table. A fluoroscopic screen is positioned in front of the patient, and the radiologist instructs him to take small swallows of the barium. A series of pictures are taken, with the patient changing position several times. If the entire small intestine is being studied, the patient is next taken to a waiting area and returns every 15 to 30 minutes for more pictures. A stomach—duodenum study takes about a half hour. The longer study takes from 1 to 3 hours.
A lower GI , often called simply a barium enema , is much more involved. It is used when there is a suspicion of diverticulitis, bowel obstruction, colon polyps, colitis, or other intestinal disorders. A strict diet is prescribed, along with laxatives, for several days before the test. Two enemas are given on the morning of the study. For this exam the patient lies down on the X-ray table. The doctor inserts a lubricated, gloved finger into the patient's rectum to make sure there are no obstructions and then inserts the enema tip. The tip has a builtin balloon that can be inflated if the patient feels unable to retain the enema, like the upper GI, an injection of glucagon is often given to counteract the feeling of “fullness” experienced by most people. The fluoroscope is then positioned and the technologist begins the enema: a solution of barium is pumped into the rectum until it fills the large intestine. Air may then be pumped into the rectum for greater contrast. Both the enema and the air can cause a feeling of fullness and discomfort. The patient retains the enema and the air until all the pictures are taken.
There is a breath test used to detect the bacterium Helicobacter pylori , which is thought to be the cause of many ulcers. The patient simply blows into a small plastic bag, then drinks a glass of clear, tasteless liquid. The liquid consists of substances that will be broken down by any H . pylori in the stomach. Thirty minutes later, the patient exhales into another plastic bag. Both bags are sent to a laboratory to be tested for H . pylori . The breath test for H . pylori bacterium is about 95 percent accurate.
The gall bladder, an organ in the upper right abdomen responsible for storing the bile necessary for fat digestion, is a frequent site of infection and may also develop stones. Examination of the gall bladder can be done with X rays, ultrasound, or nuclear imaging. Most routine gall bladder studies are done with ultrasound. An 8-hour fast is required before the test. The patient is given a gown to wear, may be asked to drink a white liquid, and then lies down on the couch. The doctor applies a special lubricant to the abdominal area and moves the transducer over it. The patient can watch the results on a monitor.
If stones develop in the gall bladder and block the flow of bile, infection results—a condition called acute cholecystitis. Nuclear imaging is considered the most specific diagnostic tool for this disorder. The patient fasts for 4 hours before the exam. An isotope is injected and the patient lies down under a gamma-ray camera. Pictures are taken every 5 to 10 minutes for a half hour and then every 15 minutes for one and a half hours.
The liver makes the bile needed for fat digestion, and the pancreas makes the enzymes necessary for fat digestion. Neither the entire liver nor the entire pancreas can be seen with X rays. X rays of the blood supply and ductal structures, however, enable the skilled specialist to make accurate assumptions about the condition of either. CT imaging can give a full picture of both organs and is safer than X rays. Ultrasound is also useful.
If the results of lab tests suggest liver disease or if the organ is enlarged, a special needle biopsy may be done. The patient is normally asked to avoid eating the night before the test. Medication by mouth or injection may be given. The gastroenterologist feels the lower edge of the liver, selects a spot, and injects a small amount of local anesthetic under the skin. Next a larger needle with a syringe is inserted. There will be pressure and even a dull pain. The plunger of the syringe is pulled back, and liver cells are extracted. The needle is then removed and pressure is applied to the puncture site.

| Kind | Function | How It Works | Time Required |
|---|---|---|---|
| Blood glucose monitoring | Measures the level of glucose (a kind of sugar) in blood | Wash your hands thoroughly. Prick a finger or earlobe to obtain a drop of blood, then follow instructions. | 1 to 2 minutes |
| Ovulation monitoring | Measures the quantity of luteinizing hormone (LH) in urine | A chemically treated strip is dipped in urine specimen and compared with a color guide. | 20 minutes to 1 hour |
| Pregnancy | Detects human chorionic gonadotropin, produced by a developing placenta, in urine | Chemicals are mixed with a urine specimen in a small test tube. A ring formation or color change indicates pregnancy. | 20 minutes to 2 hours |
| Urinary tract infections | Detects nitrite in urine | Chemically treated test strip is dipped in urine specimen on three consecutive mornings. | 30 to 40 seconds |
| Occult fecal blood | Detects hidden blood in stools | A color change, appearing when stool specimen is brought into contact with peroxide and guaiac, indicates hidden blood. | 30 seconds to 16 minutes |
| Gonorrhea | Detects the bacteria causing gonorrhea in the specimen of pus from the penis | Specimen, collected on a slide, is allowed to air-dry. Then follow directions. | Several days |
| Blood pressure | Measures the pressure of blood on the walls of the arteries | The center of a cuff is placed on the pulse point of the upper arm. With or without a microphone, the user listens for artery sounds. | 2 to 5 minutes |
| Impotence | Detects, measures the rigidity of erections during sleep | Soft fabric band or stamps are placed around the penis before the subject goes to bed at night. The strips break at different degrees of pressure. | Overnight |
| Vision | Screens for visual acuity problems | Using three different tests, you read special eye charts. | 2 to 3 minutes |
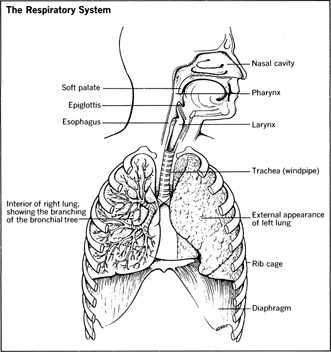
The Respiratory System
The respiratory system includes the pharynx, trachea, bronchi, and the lungs.
A chest X ray (described earlier) is usually the first test done when symptoms indicate a possible problem in the respiratory system. When the bronchi must be seen in more detail, a bronchogram may be done. This requires the suppression of the “coughing reflex” by spraying a local or topical anesthetic in the patient's mouth and back of the throat. Then a thin metal tube shaped like a candy cane (a cannula) will be placed in the mouth with the curved end over the back of the tongue. Anesthetic is injected into the cannula, which runs down the back of the throat into the bronchi. A rubber tube (catheter) is passed through the patient's nose, down the back of the throat, through the larynx, the trachea, and then into the bronchi of one or both lungs. A special dye is then instilled into the catheter, which runs down and fills the tubes. The dye highlights the bronchi, making it easier to see blockage and tight areas on the X ray.
A bronchoscopy may be in order if X rays or CT reveal potential problems and the physician needs a closer look or a tissue sample. The physician inspects the larynx, trachea, and bronchi through a flexible fiberoptic tube called a bronchoscope. Miniature instruments are fed through the bronchoscope to collect tissue samples.
A group of tests called pulmonary function tests help the physician determine if certain symptoms may be due to either restrictive or obstructive lung disease. These tests measure how much air can be forcibly exhaled after inhaling as deeply as possible, how much air remains in the lungs after a forcible exhalation, and how much air is expired with each normal breath. They evaluate how well the lungs stretch with each breath inhaled and how well they collapse with each breath exhaled.
The patient is put in a pressurized plexiglass cabin called a body box, which looks like a large phone booth. The patient's nose is closed off with a nose clip and a special mouthpiece is inserted in the mouth. Then the patient performs a series of breathing maneuvers by exhaling into the mouthpiece, which is attached to monitoring equipment. The tests take 15 to 45 minutes.
The Endocrine System
There are 7 endocrine glands that make up the endocrine system: pituitary, thyroid, parathyroids, adrenals, pancreas, ovaries (women), and testicles (men). The glands secrete hormones that produce a specific effect or regulate a certain action of other body organs. Laboratory tests of blood and urine are important diagnostic tools for the glands, and all can be visualized with X rays, CT, nuclear imaging, and ultrasound if lab tests indicate a potential problem. Some tests may necessitate the injection of a special dye to highlight the target area.
The Kidneys and the Urinary System
Laboratory tests of the urine are the most obvious way of beginning a diagnosis of kidney or urinary system problems. A resting EKG may also be done as well as nuclear imaging, ultrasound, and X rays. If a kidney biopsy is needed, the patient is normally given an anesthetic to induce drowsiness and is then instructed to lie face down on a table. The procedure is similar to that of the liver biopsy. First the anesthetic is injected, then the aspirating needle is inserted. This takes only a minute or so. An overnight stay is required for observation. Patients may experience a dull backache for several days after the biopsy.
An intravenous urography is a common test for urinary tract problems. Colon cleansing (strict diet, laxative, enemas) is often done before the test. Dye is injected into the patient's arm (or may drip in gradually from a diluted bottle of fluid). X rays are taken at timed intervals. A compression cuff (like a large blood pressure cuff) may be put around the abdomen to apply pressure just below each kidney, and more pictures are taken. The patient is then told to void his or her bladder; another X ray is taken, and the test is over.
Ears, Nose, and Throat
The otorhinolaryngologist specializes in treating problems of the ears, nose, and throat. Difficulty in hearing, faulty balance or vertigo, earache, and ringing in the ears (tinnitus) are common ear complaints. Congestion, discharge from the nose, postnasal drip, itching and sneezing, headaches over the eyes, pain over the upper teeth, and unexplained fever are complaints associated with the nose and sinuses. Laryngitis, sore throat, or difficulty in swallowing are common throat complaints.
An audiogram evaluates and measures hearing. The patient is seated in a booth and earphones are placed over the ears. A series of tones that vary in loudness are played through the earphones and the patient uses hand signals to indicate hearing a tone. Each ear is tested separately.
A tympanogram measures vibrations of the eardrum. A rubber plug is inserted in one ear and mild pressure is applied. The tympanogram reveals the type of hearing loss caused by a perforated eardrum, by an eardrum that has become thickened from an infection, or by an obstruction in the middle ear.
Patients who experience dizziness may be given an electronystagmogram , a series of neurological tests that record eye movements. Abnormal movements of the eye can indicate a problem with the balance mechanism (vestibular system). The technician tapes a small metal disk under each eye and on the bridge of the nose. These sensors are attached by lead wires to a graph machine. The patient is then instructed to follow a slowly moving target with the eyes as eye movements are recorded. In the next test the patient, with eyes closed, lies down and turns to one side. Eye movements are recorded as water is placed into the external ear canal. This procedure often produces dizziness or nausea that persists for several hours.
Smears and cultures are the common lab tests for nose and throat complaints. X ray examinations may also be done. In some cases a biopsy may be necessary. For the nose, a needle aspiration is the common method, either through the nose or upper gum of the mouth. A local anesthetic is given first. An excisional biopsy may be necessary, in which case a small piece of tissue is removed. For the throat an excisional biopsy is commonly done, normally under general anesthesia, and an overnight stay in the hospital may be required. A laryngoscope is used to obtain the sample. The throat remains sore for several days afterwards.
The Eyes
Opthalmologists are certified doctors of medicine who specialize in medical and surgical care of the eye. As such, they have the greatest range of expertise among eye-care specialists. In addition to testing vision and prescribing corrective lenses, opththalmologists diagnose and treat all eye disorders, from minor infections to conditions such as glaucoma that can lead to blindness.
Optometrists diagnose vision problems and prescribe lenses, screen for glaucoma, and identify and treat other disorders. They are not physicians, but they have completed two years of study in an approved college followed by four years at a school of optometry.
Opticians fit and sell corrective lenses prescribed by an opthalmologist or optometrist.
The common eye exam includes tests for visual acuity, color blindness, and muscle integrity. Other tests are the slit-lamp exam, tonometry, and retinal exam.
The Snellen visual acuity chart is used to measure visual acuity. Letters, numbers, or symbols are arranged in rows, each row formed by characters of the same size. The top row contains large characters, with each succeeding row formed by smaller characters. The patient is asked to stand or sit 20 feet from the chart and identify the figures line by line from top to bottom until the figures are no longer recognizable. The doctor will check each eye individually while the patient covers the alternate eye; then both eyes are tested together. This test detects errors of vision such as nearsightedness, farsightedness, and astigmatism, which are the result of defects in the size and shape of the eye. Continuing the test, the opthalmologist fits the patient with a series of corrective lenses of different strengths. The patient looks through each sample lens and reads the Snellen chart again, identifying those lenses that help him see the letters or symbols most clearly.
Color blindness is the inability to recognize one or more colors. Various charts are used to detect color blindness. One commonly used chart contains patterns of colored dots. A color blind person will not be able to distinguish between dots of certain colors and therefore will not be able to discern a design defined by these dots.
The muscle integrity exam tests eye movement to determine if both eyes can focus together. The movement of the eye toward any desired direction is controlled through the coordinated action of six muscles attached to the eyeball under the conjunctiva. For an object to be perceived properly, the eye muscles must work in unison to focus the image on the center of the retina at the back of the eye. In the muscle integrity exam, the patient is asked to look in various directions. Both eyes will move together if the muscles are working properly.
The slit-lamp microscope is used to obtain a magnified view of structures at the front of the eye—the sclera, iris, conjunctiva, cornea, and lens—which are carefully checked for signs of injury or disease. A common disorder detected by slit-lamp examination is the cataract, the clouding of the normally clear lens. The standard treatment for cataracts is surgical removal of the lens, which, in most cases, is then replaced with an artificial lens. Alternatives to an artificial lens include contact lenses or thick-lensed eyeglasses.
Glaucoma is a disease caused by inadequate drainage of the fluid within the eyeball. The resulting increase in the pressure of the fluid damages the optic nerve, leading to a gradual narrowing of the field of vision and, eventually, blindness. Glaucoma is the leading cause of blindness in the United States. An instrument called a tonometer is used to measure the pressure of fluid within the eyeball. The tonometer is placed on the pupil after a drop of anesthetic has been applied to the eye, and a gauge records the resistance of the eye to the slight pressure applied. It is recommended that this painless procedure be done for those 40 and over every 2 to 3 years, or annually if there is a family history of glaucoma.
The final test in the general eye exam is the retinal exam. The room is darkened, and the doctor uses an ophthalmoscope to look through the pupil into the back of the eye.
A common disease of the retina is macular degeneration, an age-related disorder that causes increasingly blurred central vision in the elderly. A leading cause of blindness in the United States is diabetic retinopathy, a deterioration of the blood vessels of the retina brought on by diabetes.
Diagnostic Tests and the Patient's Rights
As medical costs continue to rise, questions about the necessity of various diagnostic tests will continue to be raised. For the healthy individual, it makes little sense to undergo more than the few routine screening tests necessary for his particular age group; there is always the chance of an error that may lead to additional tests at even greater expense, not to mention the emotional trauma that a false positive could cause.
For the patient experiencing particular symptoms, or those in high risk categories, the number and kind of diagnostic tests are a concern. Batteries, or sets, of tests are a particular cause for concern. The batteries can be complex, and the physician may not take the time to explain each one in detail so that the patient thoroughly understands what they mean in terms of discomfort, risk, and cost. The value of a particular test must also be weighed against its results. Expensive CT and MRI tests are the “study of choice” for many problems, but for others, the less expensive X ray might do just as well or better. When presented with the need for diagnostic tests, then, the patient should endeavor to become as informed as possible about what is necessary. As already mentioned, having a physician with whom you can converse easily and understand is an important factor in the quality of the medical care you receive.

Comment about this article, ask questions, or add new information about this topic: