Common Surgical Procedures - Male reproductive system
Surgical procedures of the prostate, testis, scrotum, and penis are considered in this section. Undescended testicles and vasectomy are also among the subjects discussed.
Prostate Surgery
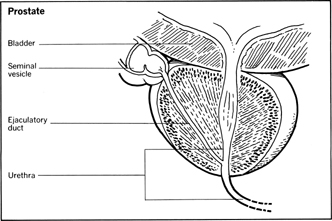
The prostate gland is a small cone-shaped object that surrounds the male urethra, the tube that carries urine from the urinary bladder to the penis. It is normally about one-half inch long and weighs less than an ounce. Ejaculatory ducts empty through the prostate into the urethra, and other ducts drain glandular secretions of the prostate into the urethra. Because of the intimate association of the prostate gland and the urinary tract, a disorder in one system can easily affect the other. A urinary infection can spread to the prostate and an abnormality of the prostate can interfere with the normal excretion of urine.
Enlargement of the Prostate
A relatively common problem is the tendency of the prostate to grow larger in middle-aged men. The gradual enlargement continues from the 40s on, but the symptoms usually go unnoticed until the man is in his 60s. At that point in life, the prostate may have become so enlarged that it presses on the urethra and obstructs the flow of urine from the neighboring bladder. The older man may experience various difficulties in emptying his bladder. He may have to urinate more frequently, and suddenly find himself getting out of bed at night to go to the bathroom. He may not be able to develop a urine stream of the size and force he had in earlier years. He may have trouble getting the stream of urine started and it may end in a dribble.
In addition to the somewhat embarrassing inconveniences caused by prostate enlargement, the urinary bladder may not drain properly and can eventually lose its own muscle tone needed for emptying. Residual urine in the bladder can become a source of infection, and backflow into the ureters can gradually affect those tissues and the kidneys. It has been estimated that 20 percent of all older men may need treatment of some kind, including surgery, for correcting this problem of the prostate gland.
Factors Indicating the Need for Surgery
Factors that may decide in favor of surgical removal of the prostate include residual urine in the patient's bladder; blood in the urine, with evidence that the blood comes from the prostate; the severity of the inconveniences associated with irregular urination; and complications such as the presence or threat of failure of the wall of the urinary bladder, the formation of stones, and symptoms and signs of infection.
Surgical Methods
There are several methods of performing a prostatectomy (excision of all or part of the prostate) for relief of the symptoms of an enlarged prostate, a condition that may appear on the patient's medical records as benign prostate hyperplasia . All of the methods are relatively safe and in none of the techniques is the entire prostate removed. One method, called transurethral resection , requires insertion of an instrument into the urethra through the penis. The instrument, a resectoscope , uses a high-frequency electric current to cut away the tissue inside the gland. This technique avoids open surgery and requires a postoperative hospital stay of only a few days.
Open Surgery
The other techniques involve open surgery , that is, surgery in which an incision is made in the pelvic or rectal area to make the prostate gland accessible so that its inner tissues can be removed. The differences in the various open surgery techniques depend upon such factors as where the incision should be made and the risks associated with the approaches. The incision is made either in the perineum , the region between the rectum and the testicles, or through the abdomen. Only a small percentage of patients experience complications or regrowth of the prostate tissues to produce a second enlargement problem. Impotence is usually not an aftereffect of the surgery, and libido is normal.
Infections of the Prostate
Infections of the prostate gland can involve obstruction of the urethra, but the problem usually can be resolved by the use of medications and techniques other than surgery. An abscess, however, may require an incision to drain the prostate. Surgery also may be recommended for the treatment of stones, or calculi, that develop in the prostate and cause obstruction or contribute to infections.
Cancer of the Prostate
Cancer of the prostate also may occur in older men, causing obstruction or the urinary flow or contributing to infection of the urinary tract. If examination including biopsy studies confirms the presence of cancer, the surgeon may recommend radical prostatectomy. In this procedure an incision is made either through the lower abdomen or through the perineum to remove the entire prostate gland and surrounding tissues, such as the seminal vesicles. Hormonal therapy, chemotherapy, and radiation treatments also may be administered.
Tumors of the Testis
Tumors of the testis occur most frequently in men between the ages of 18 and 35. Such a tumor appears as a firm and enlarged testis and usually without pain unless bleeding is involved as a symptom. Testicular tumors generally are malignant and spread rapidly to other parts of the body, including the lungs. The onset of the disorder can be so insidious that the patient may seek medical advice for a more obvious secondary problem, such as the apparent development of mammary glands on his chest, the result of disruption of his normal male hormonal balance.
Special laboratory tests and other examination techniques usually are required to determine which of several possible kinds of testicular tumors may be involved and the extent of the metastasis of the cancer cells to other body areas. If cancer of a testicle is confirmed, it is removed by an incision through the groin area, and neighboring lymph nodes also will be taken out. The surgical procedure usually is supplemented with chemotherapy and radiation. The prognosis, or chances for recovery, following surgical removal of a testicular tumor depends upon the particular kind of cancer involved and how far the disease had progressed before medical treatment was begun.
Tumors of the Scrotum and Penis
Tumors of the scrotum and penis are relatively uncommon but do occur. Cancer of the scrotum is usually associated with exposure to cancer-causing chemicals. Boys who worked as chimney sweeps a century ago tended to develop cancer of the scrotum from body contact with soot in coal-burning fireplaces. Cancer of the penis occurs usually in men who have not been circumcised. In either type of cancer, the treatment usually requires removal of the affected tissues. This can mean castration in the case of scrotal cancer or amputation of a part or all of the penis, depending upon the extent of the cancerous growth. Surgery that requires removal of a part of the reproductive system can have a devastating psychological effect on a man, but the alternative is likely to be early death from the spread of cancer.
Undescended Testicles
About 10 percent of cases of tumors of the testis occur in men with an undescended testicle. Because the chances of a tumor developing in an undescended testicle are as much as 50 times greater than the incidence for the normal male population, the existence of an undescended testicle can warrant corrective surgery.
Ordinarily, the testicles descend from their fetal location in the abdomen into the scrotum about two months before birth. But in one case in 200 male births, a child is found with a failure of one or, less commonly, both testicles to descend properly into the scrotum. In addition to the risk of cancer, undescended testicles are associated with lack of fertility and other problems, such as hernias.
Cryptorchidism
In male babies and young boys, an undescended testicle sometimes can be encouraged to enter the scrotum by manipulation or administration of hormones. Many surgeons recommend that the developmental problem of undescended testicles, or cryptorchidism , be corrected before a child enters school, although the surgical procedure for correcting the situation can be postponed until adolescence or adulthood. The operation for correcting an undescended testicle is called orchidopexy and involves an incision in the groin to release the testicle and its attached cord from fibrous tissue holding it in the abdomen. The testicle may be brought directly down into the scrotum, where it may be anchored temporarily with a suture, or it may be brought down in stages in a series of operations to permit the growth and extension of blood supply to the testis. The original location of the undescended testicle determines which procedure is used.
Vasectomy
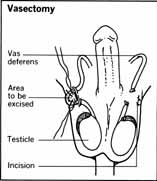
Vasectomy is a birth control technique that is intended to make a man permanently sterile. It does not involve the removal of any of the male reproductive system and does not result in a loss of potency or libido. A vasectomy is a relatively simple operation that can be performed in a physician's office in less than 30 minutes and requires only a local anesthetic. The operation is similar to but much less complicated than the procedure in which a woman may be sterilized by cutting or tying her Fallopian tubes. A vasectomy requires no hospitalization, and the man is able to return to work or other normal activities after a day or two.
How the Procedure Is Done
The vasectomy procedure requires a small incision, about one-half inch in length, on either side of the scrotum. The surgeon removes through the incision a short length of the vas deferens , the tube that carries spermatozoa from the testicles, and ties a piece of surgical thread at two points about an inch apart. Then a small piece of the vas deferens between the tied-off points is snipped out of the tube. The procedure is done on each side. With the ducts of the vas deferens cut and tied, sperm from the testicles can no longer move through their normal paths to the prostate, where they would become mixed with semen from the prostate and seminal vesicles and be ejaculated during sexual intercourse.
Sterility Is Usually Permanent
A vasectomy does not immediately render a man sterile. Sperm already stored in the seminal “pipeline” can still be active for a period of a month to six weeks, and a woman who has intercourse with a vasectomized man during that period can become pregnant. On the other hand, a man who undergoes a vasectomy should not expect that the severed ducts can be connected again should he want to become a father in the future. Sperm banks have been offered as a possible alternative for the man who might want to store some of his spermatozoa for future use, but there is little evidence that the sperm will remain fertile in a sperm bank for more than a year or 18 months. In rare cases, men who have undergone vasectomies have unintentionally become fertile again because of canalization , or creation of a new channel connecting the severed ends of the vas deferens; in one case the canalization occurred 8 years after the vasectomy was performed.
The vasectomy is regarded as an extremely safe operation, and complications are infrequent. Some swelling and discomfort are reported by a small percentage of men undergoing the operation. Steroid hormone drugs are sometimes administered to control these aftereffects.

Comment about this article, ask questions, or add new information about this topic: