Common Surgical Procedures - Abdominal region
This section discusses the following procedures or conditions: appendicitis, peptic ulcers, hiatus hernia, adhesions, cancer of the stomach and of the intestines, gallbladder surgery, inguinal hernia, and hemorrhoids.
Appendicitis
Inflammation of the appendix is one of the most common causes of abdominal surgery today, particularly among children. But appendicitis was not recognized as a disease until 1886, leading some doctors to believe that this digestive tract infection may be related to a change in eating habits that occurred within the past century. The vermiform appendix, the site of the inflammation, is a short, wormlike (or vermiform ) appendage at the junction of the small and large intestines. Its function in humans is unknown; plant-eating animals have an appendix, but carnivorous animals, like cats, do not. Humans live quite well without an appendix, so it seems reasonable to have a diseased appendix removed.
Symptoms
The appendix can cause trouble if it becomes obstructed by a foreign body, a tumor, an infection, or other cause of inflammation. Pain is a common symptom; there may be two kinds of pain at the same time: one, localized on the lower right side of the abdomen, near the site of the appendix; the other, more generalized and colicky, of the kind sometimes associated with gas in the intestine. Some patients experience diarrhea or a constant urge to defecate, an effect attributed to irritation of the bowel by the abnormal activity of the appendix. Frequently there is loss of appetite, nausea and vomiting, and a fever.
The symptoms of appendicitis may begin suddenly, but frequently take from 6 to 18 hours to develop into a pattern typical of the disease, so most cases permit ample time for a doctor to examine the patient and make a diagnosis before the problem becomes critical. During the period that any symptoms suggest a possibility of appendicitis, the patient should avoid the use of any laxatives.
Ruptured Appendix
A potentially serious complication of untreated appendicitis is rupture of the appendix, which can produce a slightly different set of symptoms because of the onset of peritonitis , a dangerous inflammation of tissues outside the intestinal tract. The contents of the ruptured appendix leak into the body cavity, spreading the bacterial infection and irritating the lining (peritoneum) of the abdominal cavity. Diarrhea and a fever of more than 101° F. are frequently associated with a perforated or ruptured appendix. The colicky pain may disappear suddenly, because the internal pressure ends with perforation of the wall of the appendix, but it is quickly replaced by the pain of peritonitis. The severe pain of peritonitis usually is made worse by any body movement, including the abdominal muscle movement required for coughing or sneezing.
Appendicitis with perforation is much more common in older persons, perhaps because the early symptoms of colicky pain that younger people notice are not felt by older people, so the disease is not detected until it has reached an advanced stage. Appendicitis also requires special attention in pregnant women, because the enlarged uterus crowds and repositions segments of the intestinal tract and the potential threat grows more serious during the last trimester of pregnancy.
Surgical Procedure
Laboratory tests usually are checked before surgery proceeds if there is no evidence of perforation. The usual symptoms of appendicitis can be produced by a number of other ailments, and the symptoms may diminish with bed rest, time, and medications. However, appendicitis must be considered in any case of acute abdominal complaints, and many surgeons and physicians follow the rule of “When in doubt, operate.” Surgery for appendicitis is fairly simple and safe if the appendix has not perforated. An incision is made in the lower right side of the abdomen, the connection between the end of the large intestine and appendix tied off with surgical thread, and the appendix cut away from the stump. The actual operation, if uncomplicated by peritonitis or other factors, may require only a few minutes. A hospital stay of a few days is usually required during which the diet is readjusted from nothing by mouth at first, to a liquid diet, then a soft diet, etc. Normal work activities usually can be resumed within two or three weeks following surgery. Complications other than those related to peritonitis are rare. In untreated cases involving peritonitis, however, the risk is very high.
Peptic Ulcers
The cause of peptic ulcers is still unknown, although the disease affects about 10 percent of the population at some time in life. Men are four times as likely as women to develop ulcers; the incidence is highest in young and middle-aged men. Peptic ulcers may occur in the stomach, where they are called gastric ulcers , or in the duodenum, where they are called duodenal ulcers . Ninety percent of the ulcer cases that reach the physician's office for treatment are in the duodenum, a short length of the small intestine just beyond the stomach. Autopsy studies indicate that gastric ulcers may be as common as duodenal ulcers, but are frequently not detected during the life of the individual.
Causes
The development of ulcers is associated with the possible action of gastric acid on the lining of the stomach and duodenum in people who may have inherited a sensitivity to the substances. Ulcers are also related to the use of certain drugs and exposure to severe burns, injury, emotional stress, and disease.
Symptoms
A common symptom is a gnawing pain in the area of the stomach from 30 minutes to several hours after eating; the pain is relieved by food or antacid medications. The pain sometimes is likened to heartburn and may be described as radiating from the abdomen to the back. Some patients report the discomfort is more like a feeling of hunger or cramps; they may be awakened from sleep by the feeling that is relieved by a midnight snack of milk or other foods. Attacks of ulcers may be seasonal, occurring in certain patients only in the spring and autumn. In severe cases there may be bleeding without any sensation of abdominal pain; bleeding occurs from erosion of the lining of the stomach or duodenum and penetration of blood vessels in those membranes.
Complications other than bleeding can include perforation of the wall of the stomach or duodenum by continued erosion, or inflammatory swelling and scarring by an ulcer at a narrow part of the digestive tract, causing an obstruction. A duodenal ulcer can erode into the head of the pancreas, which secretes its digestive juices into the small intestine in that area. The pain may then become more or less continuous regardless of efforts to palliate it with food or antacids.
Symptoms vary only slightly between duodenal and gastric ulcers. Gastric ulcer pain usually begins earlier after a meal, attacks generally last longer, and symptoms, including vomiting and loss of appetite, may be more severe than in duodenal ulcer. But because of the similarities, physicians usually rely on laboratory tests and X-ray studies to determine the precise location in the digestive tract of the peptic ulcer.
Duodenal Ulcers
Duodenal ulcers nearly always occur within an inch of the pyloric valve separating the stomach from the small intestine. The pain or discomfort follows a cycle. The patient may experience no pain until after breakfast. The pain is relieved by the noon meal but returns in the afternoon and occurs again in the evening. Milk or other bland food or medications relieve the pain that may appear at various times in the cycle. The symptoms of duodenal ulcers also go through periods of remission and recurrence over months or years. Most duodenal ulcers are treated with diet, drugs, and measures that encourage rest and relaxation.
Surgical Procedures
Surgery for either duodenal or gastric ulcer is designed to reduce gastric acid secretion rather than simply to excise the ulcer from the normal digestive tract tissue. One surgical approach, called subtotal gastrectomy , involves cutting away a portion of the stomach in the area where it joins the duodenum. There are several variations of this technique, including one in which the remaining portion of the stomach is attached to the jejunum, a segment of the small intestine. The ulcerated portion of the duodenum may be removed during the reconstructive surgery of the digestive tract, or it may be left in the duodenal segment that is closed during the gastrectomy procedure. An interesting effect is that a duodenal ulcer usually heals, when left in place, after the gastric juices are routed into the intestine through the jejunum. The reconstructed stomach and stomach-to-intestine connection cause no serious problems in eating after the patient has recovered.
A second surgical approach, called a vagotomy , involves cutting a part of the vagus nerve trunk that controls the secretion of stomach acid. There are several variations of vagotomy, each technique affecting a different portion of the vagus nerve distribution to the stomach.
Gastric Ulcers
Stomach or gastric ulcers tend to develop in older persons more often than duodenal ulcers, and the problem seems to be less importantly related to the overproduction of gastric acid. The real hazard of stomach ulcers is that a significant percentage are found to be a kind of cancer and do not respond to the usual therapies for controlling peptic ulcer symptoms. If it is determined that a stomach ulcer is a malignant growth, a partial gastrectomy is performed in the same manner as an operation of the type for duodenal ulcers. The vagotomy approach is not used for treatment of a stomach ulcer unless the ulcer is excised at the same time.
Hiatus Hernia
The term hiatus hernia actually describes a diaphragmatic hernia or weakness in the diaphragm, the horizontal muscular wall separating the organs of the chest from the organs of the abdomen. A hernia is an abnormal protrusion of an organ or tissue through an opening. A hiatus , or opening, occurs naturally to permit the esophagus to carry food from the mouth to the stomach. Blood vessels and nerves also pass through the diaphragm. The diaphragm is an important group of muscles for contracting and expanding the lungs, forcing air in and out of the lung tissues.
Hiatus hernias are rare in children, but as people grow older, there may be a weakening of the diaphragm muscles and associated tissues. Aided by a tendency toward obesity and the use of girdles and other tight garments, a portion of the stomach may be pushed through the opening designed by nature for use of the esophagus. Aside from the discomfort of having a part of the stomach in the chest, there are potential dangers of incarceration of the stomach, with obstruction, strangulation, and hemorrhage with erosion of the stomach lining. In severe complications, the entire stomach along with intestines and other abdominal organs may be forced through the hiatus hernia into the chest area.
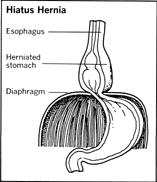
The most common kind of hiatus hernia is sometimes called sliding hiatus hernia from the tendency of the stomach to slide in and out of the thorax, or chest cavity, when the patient changes body positions or as a result of the pressure of a big meal in the gastrointestinal tract. Sometimes the herniated stomach does not move at all but remains fixed, with a significant portion of the stomach above the diaphragm. Hiatus hernia causes heartburn symptoms, including regurgitation of digested food and gastric acid from the stomach, when one is lying down or straining or stooping. The effect also may be noticeable in a woman during pregnancy.
Nonsurgical Treatment
Many cases of hiatal hernia can be treated without surgery through a change of eating habits and the use of antacid medications. The patient may be advised to eat small amounts more frequently during the day with dietary emphasis on high-protein, low-fat foods. Some physicians recommend that patients use liquid antacid medications rather than antacid tablets or lozenges.
Surgical Treatment
When surgery is recommended to correct hiatus hernia, the repair may be performed either through the abdominal wall or through the chest. About three-fourths of the procedures are handled through abdominal incisions, because surgeons often find other abdominal problems that need to be corrected at the same time, such as peptic ulcers or gall bladder disease. The opening through the diaphragm is firmly closed with sutures to prevent upward movement of the stomach. The stomach and lower end of the esophagus may be anchored in place in the abdomen. The chances of recurrence are about one in ten, although some patients may continue to have a few of the symptoms of the disorder for a while after the hernia repair.
Adhesions
Adhesions may develop between various abdominal organs and the peritoneum, the membrane lining the abdominal cavity. The bowel may acquire adhesions that result in obstruction of the intestinal tract. Adhesions may form between the liver and the peritoneum or between the liver and the diaphragm. The symptoms may be pain or cramps in the area where tissues are literally stuck together; in more serious cases that involve bowel obstruction, symptoms may include constipation, vomiting, and distension of the abdomen. Adhesions do not show on X-ray film and can be difficult to diagnose unless the patient's medical history suggests a cause for the bands or filaments of tissues responsible for the adhesions.
Causes
The causes may be peritonitis, injury, infection, internal bleeding, or foreign objects. Adhesions occur after an operation, perhaps because of a bit of blood resulting from surgery or as a result of a speck of talc from the surgeon's glove or a fiber from a surgical drape which produces a foreign-body reaction, much like an allergic reaction, when it comes in contact with abdominal tissues. Disease organisms may enter the female abdominal cavity through the Fallopian tubes to produce adhesions, especially in the case of gonorrhea, which can escape early detection in women because of the lack of obvious symptoms.
Complications
Adhesions can cause complications, such as changing the position of the intestinal tract through twisting or otherwise distorting its path so that bowel movements are obstructed. If the involved portion of the intestine becomes so seriously damaged that it no longer functions properly, the surgeon may have to remove that section. Generally, when the surgeon is correcting the problem of adhesions, a relatively simple procedure of cutting away the tissue bands or filaments holding organs in abnormal ways, he inspects the organs to determine if they appear to be in good working order. That part of the operation may add 15 or 20 minutes to the time spent on an operating table, but it helps insure that the patient will not have to be returned soon for further surgery.
Cancer of the Stomach
There are several possible types of stomach tumors, but one kind, called adenocarcinoma , is one of the greatest killers of men over the age of 45. Although the incidence of stomach cancer in the United States has declined considerably since the end of World War II, the death rate from this problem in the United States alone is about 15,000 per year. In central and eastern Europe the incidence of stomach cancer is about four times, and in Japan seven times, that of the United States. Almost two-thirds of the stomach cancers develop near the pylorus, the opening from the stomach into the small intestine; only five percent involve the entire stomach area.
Symptoms
Symptoms include a feeling of heaviness rather than pain following a meal. The patient in many cases mysteriously loses his appetite for meat and begins to lose weight. There may be vague symptoms of an upset stomach, with some vomiting, especially if the tumor begins to obstruct the pylorus such that stomach contents cannot be emptied into the intestine. The vomitus usually is the color of coffee grounds, suggesting a loss of blood from the stomach lining because of the tumor, and the patient's stools also may be dark in coloration because of internal bleeding. The physician frequently can confirm his suspicions about the cause of the symptoms by laboratory analysis of a specimen of cells from the stomach, by X-ray studies of the stomach, or by an examination with a gastroscope that permits a direct view of the interior of the stomach. In some cases the physician will be able to feel an abnormal mass in the stomach by palpating the stomach area of the abdomen with his hands.
Treatment
Treatment is by cutting away the tumor and surrounding tissues that may be involved, including parts of neighboring organs. The lymph nodes in the region of the stomach are also removed. The remaining part of the stomach is used to build a new digestive organ, as in a case of partial gastrectomy for correcting a peptic ulcer problem. However, before beginning reconstructive surgery, the physician usually orders biopsy tests of the remaining tissues to make sure the new stomach will not be made of tissues in which tumor cells have spread. If the edges of the remaining stomach wall are found to contain tumor cells, the surgeon simply extends the area to be removed. As in subtotal gastrectomy for peptic ulcers, the remaining portion of the stomach may be connected directly to the upper portion of the small intestine, at the duodenum or the jejunum.
Meals are provided in the form of intravenous feedings for the first few days following surgery. Sips of water may be permitted on the second or third day after the operation with the amounts gradually increased to one or two ounces of water per hour as the new digestive system adjusts to fluid intake. Then soft or bland foods can gradually be taken orally in a half-dozen small feedings each day. It may take three or four months for the new stomach to distend and adjust to normal eating habits of the patient.
Postoperative Effects
Some patients may experience a variety of symptoms ranging from nausea to cramps and diarrhea while recovering from stomach surgery. The symptoms form what is known as the dumping syndrome , which occurs within a half hour after a meal, presumably by rapid distension of the upper portion of the small intestine as fluid rushes, or is dumped, into that part of the digestive tract from the new stomach. The effects can be controlled by a change of diet to eliminate starches and sugars, by delaying the intake of fluids until after the meal, by medications, and by training the patient to lie in a recumbent or semire-cumbent position to lessen discomfort following a meal. The symptoms occur in only a small proportion of stomach surgery patients, and they usually diminish gradually during the period of recovery.
Cancer of the Intestines
Small Intestine
Tumors of the small intestine are not common, but they also are not rare. It has been estimated that less than five percent of all tumors of the gastrointestinal tract occur in the small intestine. Of tumors that do develop in this portion of the gastrointestinal tract, about 90 percent are benign, or non-cancerous, growths. The symptoms of small intestine tumors may include bleeding, obstruction, and perforation of the intestinal wall. However, most tumors of the small intestine produce no symptoms at all. When tumors are found in the small intestine they usually are found at the same time in other parts of the body, and usually in a patient over 40 years of age, although the more malignant growths can occur in younger persons. Treatment of a cancer of the small bowel is by removing the affected section and administration of radiation therapy for certain kinds of cancerous tumors.
Large Intestine
Tumors of the large intestine, unlike those of the small bowel, account for a large proportion of cancers of the human body and for most of the malignant growths of the entire gastrointestinal tract. More than 40,000 deaths each year in the United States are a result of cancers of the colon and rectum portions of the large bowel. And about three-fourths of all large-intestine tumors develop near the rectal portion of the bowel, where, ironically, they should be easily available for detection during physical examination.
Tumors of the large intestine can be found in persons of any age, but they occur most frequently in patients who are of middle age or older, reaching a peak of incidence around the age of 65. Men are more likely to develop cancer of the rectum, but women are more frequently affected by cancer of the colon. While cancer of the large intestine tends to occur among members of the same families at a rate that is two or three times the normal incidence, it is believed that family environment factors, such as life style and diet, are the causative influences, rather than hereditary factors. People who develop cancer of the large intestine usually eat foods that are low in cellulose and high in animal fats and refined carbohydrates.
Bowel cancers appear to grow in size at a very slow rate, doubling about once every 20 months, so a number of years may elapse between the start of a bowel tumor and the appearance of signs or symptoms of cancer.
Symptoms
The location of the growth can influence the types of symptoms experienced. Cancer in the right colon may be found as an abnormal mass during a physical examination by a physician after complaints of fatigue and weakness and signs of anemia. The tumor can develop to a rather large size without producing signs of blood in the stools. Cancer in the left colon, by contrast, may be found after complaints of alternate periods of constipation and frequent urge to defecate, pain in the abdomen, and stools marked by dark and bright red blood. When the cancer is in the rectum, the patient may find blood mixed with the bowel movements but experience no pain in the early stages. Other symptoms of cancer of the large intestine may mimic those of appendicitis, hemorrhoids, peptic ulcer, or gall bladder disease.
As noted above, most cancers of the large bowel are close enough to the end of the intestinal tract to be observed directly by palpation or the use of fiberoptic instruments, such as a sigmoidoscope or colonoscope, which can be inserted into the rectum or colon. Biopsy samples can be removed for study and X-ray pictures taken after administration of a barium enema, which coats the bowel membrane in such a way that abnormal surfaces are clearly visible.
Surgical Procedures
Surgical procedures for treatment of cancer of the large intestine vary somewhat according to the location of the growth, but the objective is the same: to remove the affected portion and reconstruct the bowel so that normal digestive functions can resume. Radiation therapy and chemotherapy may be used in the treatment of certain advanced cases. When surgical treatment is begun soon after the first symptoms are diagnosed, the chances of curing cancer of the large bowel are very good.
If there are complications, such as obstruction of the portion of the large intestine, the surgery may be conducted in a series of stages over a period of several weeks. The several stages involve a colostomy procedure in which an opening is made in the wall of the abdomen to permit a portion of the intestinal tract to be brought to the surface of the body. After the complicating problem is treated and resection of the cancerous segment is completed, the colostomy is closed by sewing the open end of the bowel to the remaining portion and closing the opening in the abdomen.
Preoperative Steps
Some special preoperative measures are ordered for patients awaiting surgery for treatment of bowel cancer. They consist primarily of several days of liquid diets, laxatives, and enemas to make the interior of the intestinal tract as clean as possible. Other measures will be directed toward correction of anemia and compensation for possible loss of blood resulting from the cancer's invasion of bowel tissues.
Gallbladder Surgery
Gallbladder disease is one of the most common medical disorders in the United States. It has been estimated that more than 15 million Americans are affected by the disease and about 6,000 deaths a year are associated with it. The incidence increases at middle age; 1 of every 5 women over the age of 50 and 1 of every 20 men can expect to be treated for gallbladder symptoms. Approximately 1,000 people in the United States enter operating rooms each day for removal of gallstones, a primary cause of the symptoms of the disorder.
Gallstones
Gallstones generally are formed from crystals of cholesterol that gradually increase in size in the gallbladder; some, however, are formed from other substances, such as bile salts and breakdown products of red blood cells. Because they are very small in size, the stones may produce no symptoms at first. But as they grow in size they become more threatening and eventually can block the normal flow of bile from one of the bile ducts emptying into the intestine. Bile contains substances needed by the body to digest fats in the diet.
Symptoms
A common symptom of chronic cholecystitis , or gallstone disease, is a pain that appears suddenly in the upper abdomen and subsides slowly over a period of several minutes to several hours. The pain may occur after a meal or with no apparent relationship to meals. There can be tenderness in the upper right side of the body, with pain extending to the shoulder. The pain also can appear on the left side or near the center of the upper abdomen, producing misleading symptoms suggesting a heart attack. Nausea, heartburn, gas, indigestion, and intolerance to fatty foods are among other possible symptoms. The gallbladder attacks may occur frequently or there may be remissions (periods without symptoms) lasting for several months or years.
A careful and extensive physical examination, including X-ray studies of the gallbladder area, may be needed to confirm the presence of gallstones. Until recently, the most commonly used test was the oral cholecystogram (OCG), in which the patient swallowed an iodine-based “dye,” or contrast agent. X rays taken about 12 hours after administration of the dye might or might not provide useful “pictures” of the gallstones. As a result, ultrasound has largely replaced X rays as a primary test for suspected gallstones.
Acute Cholecystitis
About three-fourths of the cases of acute cholecystitis are patients who have had previous attacks of gallstone disease. In the acute phase there is persistent pain and abdominal tenderness, along with nausea and vomiting in many cases and a mild fever. Complications may include perforation, or rupture, of the gallbladder, leading to peritonitis, or development of adhesions to neighboring organs such as the stomach or intestine.
Treatment
Surgical treatment of chronic or acute cholecystitis is basically an elective procedure that can be scheduled at a time convenient to the patient. But acute cases with complications may require emergency operations. The patient can usually be maintained, after surgery, on intravenous fluids and pain-killing medications.
In gallstone surgery, the abdomen is opened so that the surgeon can examine the gall bladder and the ducts leading from it for stones. The gallbladder may be freed of stones and a temporary drainage tube inserted, with an opening to the outside of the upper abdomen. But usually the surgeon removes the entire gallbladder in an operation called a cholecystectomy . The bile duct, which remains as a link between the liver and the small intestine, gradually replaces the gallbladder in function. Conventional cholecystectomies are rarely performed now. The less invasive laparoscopic cholecystectomy has almost completely replaced the conventional surgical removal of diseased gallbladders. In the innovative method, a laparoscope removes the entire gallbladder and any stones it contains. Using videoscope surgery, everything is neatly pulled through tiny incisions in the abdomen.
A number of alternatives to surgery have been developed. A gastroenterologist may use an endoscope on older patients or those in poor health. The endoscope, a tube inserted through the chest wall, enables the physician to view the gallbladder's duct area and to widen its opening so that small gallstones can slip through the small intestine. Using a small basket on the endoscope, the physician can sometimes catch and withdraw or crush the stones.
Other nonsurgical treatments include chemical preparations. Chenodeoxycholic acid, or chenodiol, has been given orally to dissolve smaller, floating cholesterol stones. But the drug has little effect against pigment stones or stones with a high calcium content, and can cause diarrhea as a side effect.
Among the most advanced techniques is choledocholithotripsy , a non-surgical method using shock waves to destroy gallstones. Already in use as a method of shattering kidney stones, lithotripsy requires only a local anesthetic and the recovery period lasts only a few days. The physician uses a hollow tool—the lithotriptor—that is inserted through the patient's chest until it approaches the stones. With a foot switch, the physician then triggers a jolt of high-voltage, low-current electricity that shatters the stones.
In another advance, drugs have been utilized to dissolve gallstones. A drug called methyl tertbutyl ether (MTHE) has been found to break down gallstones as large as golf balls. Still partly experimental, the compound could replace most surgical operations for gallstones.
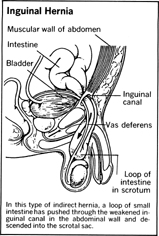
Inguinal Hernia
An inguinal hernia (hernia of the groin) can develop in either men or women at almost any age from infancy to late adult years. But the incidence of inguinal hernia is much more common in males. An inguinal hernia is one in which the intestinal tract protrudes through the opening of one of the inguinal rings on either side of the groin. In males, the inguinal rings are temporary openings through which the testicles descend into the scrotum before birth; in females, the openings permit the passage of a ligament supporting the ovary.
Causes
Normally, the inguinal rings are closed after the birth of the child. However, they may fail to close completely or the muscles and connective tissues may become stretched or weakened in later years to permit a portion of the abdominal contents, usually part of the intestine, to protrude. A number of factors can contribute to the development of a hernia, including physical strain from exercise or lifting, straining over a bowel movement, coughing spells, pregnancy, pressure of abdominal organs, or obesity.
Reducible and Irreducible Hernias
The hernia may be reducible , that is, the bulge in the abdominal wall may disappear when the body position is changed, as in lying down, only to reappear upon standing. An irreducible hernia does not allow the hernia sac contents to return to the abdominal cavity; an irreducible hernia also may be called incarcerated , a term aptly describing the hernia as being trapped. A serious complication is strangulation of the hernia contents, which usually involves obstruction of normal blood flow and resulting damage or destruction of the incarcerated intestines. A strangulated hernia may be life-threatening because of the possibility of gangrene in body tissues damaged by incarceration.
Surgical Procedure
Some hernias are called direct , some indirect , for purposes of medical records. These terms indicate to the surgeon specific layers of muscle and connective tissue that have been breached and are of no real significance to the patient, because the surgical repair procedures are essentially the same for either type. In the absence of complications, the operation is fairly simple and usually can be performed with either a general or a local anesthetic. An incision is made in the lower abdomen in the area of the hernia, the protruding organ is returned to its normal position, and the weakened or ruptured layers of muscle and connective tissue are repaired and reinforced to provide a strong internal wall that will hold the abdominal contents in place. In some cases the surgeon will use available tissues from the patient's own body in building a new wall against future hernias. The surgeon also may use a variety of materials, including silk, catgut, stainless steel, tantalum mesh gauze, or mesh screens made of plastics, in building a new barrier.
Recovery
The hospital stay for hernia repair is relatively brief, usually from three days to a week; some healthy children undergo surgery early in the morning and return home in the evening of the same day. The patient usually is instructed to avoid exercise or exertion for a couple of weeks and can return to work in a month to six weeks, depending upon the work load expected. Hernias tend to recur in only a small percentage of cases among adults and very rarely in children.
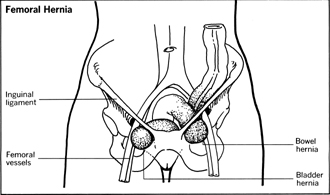
Femoral Hernia
About five percent of all hernias of the groin area are femoral hernias, with the hernia bulge appearing along the thigh. Femoral hernias occur about four times as frequently among women and usually appear in middle age. While a femoral hernia is not necessarily limited to obese patients, it is more likely to be associated with being overweight, and the movement of a bowel segment or the urinary bladder into the hernia frequently is preceded by a fat pad—a mass of fatty tissue. Femoral hernias are more prone to incarceration and strangulation than inguinal hernias. The surgical treatment of femoral hernias is similar to that used in the repair of inguinal hernias, although the incision may be made through the thigh in a few cases.
Hemorrhoids
Hemorrhoid , a term derived from Greek words meaning “blood flowing,” refers to a system of arteries and veins that serve the rectal area. The medical problem known as hemorrhoids , or piles , is a tortuous enlargement of the hemorrhoidal veins, a problem similar to the varicose veins of the legs. Causes of the varicosities of the hemorrhoidal veins include the human peculiarity of standing and walking in an erect posture—animals that walk on all fours do not get hemorrhoids.
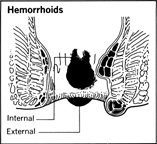
Women during pregnancies are particularly subject to hemorrhoidal problems because of the pressure on the veins of the lower body area. Other causes are constipation and straining at stool; diseases of the digestive tract resulting in anal infection; and cirrhosis of the liver, which obstructs blood flow and puts increased pressure on the hemorrhoidal veins.
Symptoms
Symptoms usually include bleeding, which may stain the patient's clothing; irritation and discomfort, including itching, in the anal region; and occasionally pain with inflammation. Because rectal bleeding also can be a sign of a number of other diseases, the physician usually makes a thorough examination to rule out other possible causes, such as cancer or ulcerative colitis.
Treatment
If the hemorrhoids do not warrant surgery, medical treatments may be prescribed. Prolapsed hemorrhoids (veins that protrude from the anus) can be reduced by gentle pressure. Bed rest, warm baths, and medications are also a part of medical treatments. A type of injection chemotherapy sometimes is used to control bleeding and eliminate the varicosed veins.
Surgery can be used to excise all the affected tissues, and the disorder also can be treated by cryosurgery in which the hemorrhoids are destroyed by a probe containing supercold liquid nitrogen or carbon dioxide. The patient usually is able to recover and return to work within one or two weeks after surgical removal of the hemorrhoidal tissues.

Comment about this article, ask questions, or add new information about this topic: