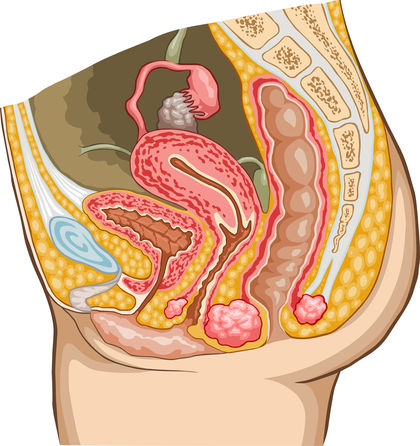
The Urinary System - Workings: how the urinary system functions
The urinary system is not the sole system in the body concerned with excretion. Other systems and organs also play a part. The respiratory system eliminates water vapor and carbon dioxide through exhalation (the process of breathing out). The digestive system removes feces, the solid undigested wastes of digestion, by a process called defecation or elimination. The skin (the integumentary system; see chapter 4) also acts as an organ of excretion by removing water and small amounts of urea and salts (as sweat).
Through its primary role of forming and eliminating urine, the urinary system also helps regulate blood volume and pressure. In addition, it regulates the concentrations of sodium, potassium, calcium, chloride, and other mineral ions (an ion is an atom or group of atoms that has an electrical charge) in the blood. These combined actions by the urinary system help the body maintain homeostasis or the balanced state of its internal functions.
Formation of urine
Urine is the fluid waste excreted by the kidneys. It can range in color from pale straw to amber (the deeper the color, the more concentrated the urine). Fresh urine is sterile (meaning it contains no bacteria) and has very little odor. Some drugs, vegetables (such as asparagus), and various diseases alter the normal smell of urine. Water forms approximately 95 percent of urine; the remaining 5 percent is made up of urea, creatinine, uric acid, and various salts.
Urea, creatinine, and uric acid are nitrogen-containing compounds produced as wastes during cellular activity. When cells break down amino acids, they produce ammonia as a waste product. Ammonia is very toxic to the body's cells, so the liver combines ammonia with carbon dioxide to create the less toxic urea, the most abundant of the nitrogen-containing wastes. Creatinine is produced when skeletal muscle cells break down the compound creatine to generate energy for muscle contraction. Uric acid, which forms only a small portion of the urine, is a normal waste product of the breakdown of nucleic acids (complex organic molecules found in living cells).
Urine is formed in the kidneys as a result of three processes: filtration, reabsorption, and secretion. Filtration takes place in the renal corpuscles; reabsorption and secretion take place in the renal tubules.
FILTRATION. Filtration is the movement of water and dissolved materials through a membrane from an area of higher pressure to an area of lower
pressure. In the body, the pressure of blood in the capillaries is higher than the pressure of the interstitial fluid, or the fluid surrounding the body's cells. Thus, through filtration, blood plasma (fluid portion of blood) and nutrients such as amino acids, glucose, and vitamins are forced through the capillary walls into the surrounding interstitial fluid to be used by the cells.
The pressure of the blood in the glomeruli is higher than in other types of capillaries in the body. This high pressure forces plasma, dissolved waste substances, and small proteins out of the glomeruli and into the Bowman's capsules. The process is called glomerular filtration. Blood cells and larger proteins are too large to be forced out of the glomeruli, so they remain in the blood. The pressure in a Bowman's capsule is low and its inner membrane is permeable, so the material that filters out of a glomerulus passes into the capsule. The fluid and material in a Bowman's capsule is referred to as renal filtrate, which is very much like blood plasma, except it contains very little protein and no blood cells.
REABSORPTION. In an average twenty-four-hour period, the kidneys form 160 to 190 quarts (150 to 180 liters) of renal filtrate. Normal urinary output in that same time frame is only about 1.1 to 2.1 quarts (1 to 2 liters). Many factors (such as increased water intake or increased sweating) can significantly alter that output amount. Nonetheless, it is quite obvious that most of the renal filtrate does not become urine, but is reabsorbed or taken back into the blood. This is important because renal filtrate contains many useful substances—water, glucose, amino acids, and mineral ions—that are needed by the body.
Reabsorption is the return of water and other substances from the filtrate to the blood. The process begins as soon as the filtrate enters the renal tubule. Cells lining the tubule actively take up useful materials (such as glucose, amino acids, vitamins, proteins, and certain ions), move them through their cell bodies, then release them into the interstitial fluid outside the tubule.
As these materials collect in the interstitial fluid, water in the tubules is drawn out through the process of osmosis. Osmosis is the diffusion of water through a semipermeable membrane from an area where it is abundant to an area where it is scarce or less abundant. Once in the interstitial fluid, the materials and water then diffuse into or enter nearby capillaries, which empty into the renal vein.
The reabsorption process is selective. The cells of the renal tubules have been "programmed" to retain substances that are useful to the body, not those substances that are of no use (such as urea and uric acid). Also, the amount of a substance that is reabsorbed is dependent on its concentration in the blood. If it exists in a low concentration in the blood, a large amount of it will be reabsorbed from the renal tubules. Conversely, if it already exists in a high concentration, very little of it will be reabsorbed into the blood.
SECRETION. Secretion is the transport of materials from the interstitial fluid into the renal filtrate. It is essentially reabsorption in reverse. The process is important for getting rid of substances not already in the filtrate. Waste products such as ammonia, some creatinine, and the end products of medications move from the blood in the capillaries around the renal tubules into the interstitial fluid. They are then taken in by the cells of the tubules and deposited into the renal filtrate to be eliminated in the urine.
Hormones and the composition of urine
Hormones are chemical "messengers" secreted by endocrine glands that control or coordinate the activities of other tissues, organs, and organ systems in the body. Each type of hormone affects only specific tissue cells or organs, called target cells or target organs. Most hormones are composed of amino acids, the building blocks of proteins. The smaller class of hormones are steroids, which are built from molecules of cholesterol (fatlike substance produced by the liver).
The hormones that affect the urinary system help it regulate the amount of water and mineral ions in urine. By extension, this action also regulates the pressure in the bloodstream and the concentration of mineral ions in the blood.
Excessive water loss in the urine is controlled by the antidiuretic hormone (ADH), which is released by the pituitary gland (a small gland lying at the base of the skull). If an individual perspires a lot, fails to drink enough water, or loses water through diarrhea, special nerve cells in the hypothalamus (a region of the brain controlling body temperature, hunger, and thirst) detect the low water concentration in the blood. They then signal the pituitary gland to release ADH into the blood, where it travels to the kidneys. With ADH present, the renal tubules are stimulated to reabsorb more water from the renal filtrate and return it to the blood. The volume of water in the urine is thus reduced, and the urine becomes more concentrated. Harmful substances are still eliminated from the body, but necessary water is not.
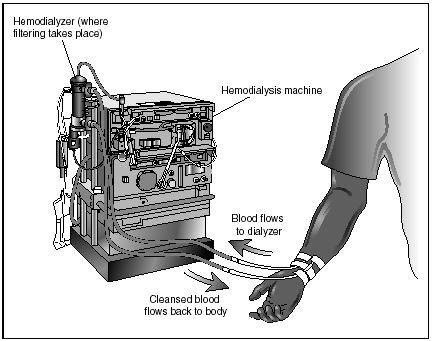
In 1950, Ruth Tucker, a forty-nine-year-old American woman, was dying from chronic kidney failure. American surgeon Richard Lawler of Loyola University in Chicago transplanted a kidney from a cadaver (dead body) into Tucker. Although her body rejected the new kidney after only a short time, Tucker became the first human to survive an organ transplantation.
With the development of immunosuppressant drugs (those that hinder the body's immune response to "foreign" tissue), the success of kidney transplants has risen. Today, individuals who receive a kidney transplant from a living donor (who is often a close relative) have a survival rate of 80 percent.
The action of ADH also controls blood volume and pressure. As more water is removed from the urine and transported into the bloodstream, blood volume and pressure increase. This is an important safeguard against low blood volume and pressure, which might be brought about by an injury.
On the other hand, if an individual takes in too much water, production of ADH decreases. The renal tubules do not reabsorb as much water, and the volume of water in the urine is increased. Alcohol and liquids containing caffeine (coffee, tea, and cola drinks) inhibit ADH production (these substances are called diuretics). Large amounts of urine are consequently excreted from the body and blood pressure decreases. If that fluid is not replaced, an individual may feel dizzy due to low blood pressure.
Another hormone that helps to control blood volume by acting on the kidneys is aldosterone. Aldosterone is a steroid hormone secreted by the adrenal cortex (the outer layer of an adrenal gland, which sits like a cap on top of a kidney). A decrease in blood pressure or volume, a decrease in the sodium ion level in blood, and an increase in the potassium ion level in blood all stimulate the secretion of aldosterone. Once released, aldosterone spurs the cells of the renal tubules to reabsorb sodium from the urine and to excrete potassium instead. Sodium is then returned to the bloodstream. When sodium is reabsorbed into the blood, water in the body follows it, thus increasing blood volume and pressure.
The kidneys themselves play a role in regulating blood pressure. When blood pressure around the kidneys decreases below normal, the cells of the renal tubules react by secreting the enzyme renin (an enzyme is a protein that speeds up the rate of chemical reactions). Renin, in turn, stimulates an inactive blood protein to change into a hormone that causes blood vessels to constrict or narrow, which immediately raises blood pressure.
Elimination of urine
The process of eliminating urine from the urinary bladder is known as urination. It is also called micturition or voiding. The sensation of having to urinate usually occurs after the urinary bladder has filled with about 7 ounces (200 milliliters) of urine. The bladder has stretched enough at this point to activate receptors within its walls. Once activated, these receptors send impulses to the spinal cord, which sends impulses back to the bladder, causing it to contract. The internal urethral sphincter (surrounding the opening of the urethra) relaxes and urine is forced into the upper portion of the urethra. This initiates the "feeling" of having to urinate.
Urination occurs when an individual voluntarily relaxes his or her external urethral sphincter. Urine flows through the urethra and the bladder is emptied. Babies do not exert control over their external urethral sphincter and urine is automatically forced out of the body when it reaches a certain level. As children mature, they learn to control their external urethral sphincter, retaining their urine until it is appropriate to urinate.
If the external urethral sphincter is not relaxed, urine will continue to accumulate in the bladder. When it reaches a volume over 1 pint (475 milliliters), the pressure created will cause pain and the external urethral sphincter eventually will be forced open, regardless of an individual's desire.

Comment about this article, ask questions, or add new information about this topic: