The Digestive System - Workings: how the digestive system functions
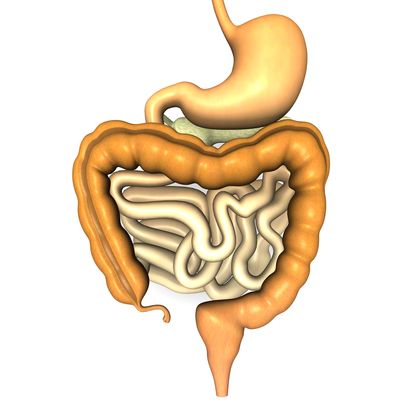
The digestive system breaks down food into a useful form through mechanical and chemical means. Mechanical digestion is the physical breaking up food into small pieces, such as by chewing. The smaller pieces are then acted upon by digestive enzymes, which change complex chemical molecules into much simpler molecules the body can easily utilize. This process involving enzymes is called chemical digestion.
Digestive activities in the mouth
Food taken into the mouth is broken down by both mechanical and chemical means. Through the process of mastication or chewing, teeth physically break down the tough tissues of meats and fibers of plants into smaller particles. The tongue helps move the food around the mouth, allowing the different sets of teeth variously to cut, tear, or grind the food. The jaw muscles, perhaps some of the strongest muscles in the body, help the teeth break down food in seconds.
Stimulated by the presence of something in the mouth, salivary glands secrete an increased amount of saliva (the sensations of sight, taste, and smell also increase saliva flow). As saliva is mixed with the food, salivary amylase (an enzyme in saliva) begins the chemical digestion of carbohydrates or starches, changing them into the simple sugar maltose.
As the food is broken down into pieces by the teeth and mixed with saliva, the tongue rolls these pieces into a battered, moistened, soft mass or ball called a bolus. Only after food has been compacted into a bolus of proper texture and consistency can swallowing occur.
Swallowing
Swallowing is both a voluntary and involuntary action. Once food has been properly chewed and mixed with saliva to create a bolus, the tongue forces the bolus toward the back of the mouth and into the pharynx. This a voluntary action; the individual has total control over moving the bolus while it is in the mouth. When the bolus presses against the soft palate, the soft palate and the uvula rise to close off the nasal passages to prevent the bolus from entering them.
Once the bolus enters the pharynx, swallowing becomes an automatic reflex action and cannot be stopped. The larynx, the upper part of the trachea that contains the vocal cords, rises. As it does so, a flaplike piece of tissue at the top of the larynx, the epiglottis, folds down to cover its opening. This prevents the bolus from passing into the trachea.
Sometimes, when a person laughs or talks while eating or drinking, the uvula and the epiglottis may not cover their openings quickly enough. If the uvula does not rise in time, bits of food or liquid may squirt up into the nose. If the epiglottis does not fold down, bits of food or liquid may enter the trachea, causing the person to cough (a protective reflex) until the food or liquid is expelled from the trachea.
Once material reaches the esophagus, the circular muscles in the walls of the esophagus begin alternately to contract and relax in a wavelike manner, pushing the bolus farther and farther down. This series of wavelike muscular motions is known as peristalsis (or peristaltic contractions). Material is pushed down the esophagus regardless what position a person is in: standing up, sitting, lying down, or upside down. Gravity helps move the bolus along, but peristalsis occurs even in the zero gravity of space.
A typical moist bolus takes about 9 seconds to travel through the esophagus. Drier boluses take longer. Liquids often pass through this muscular tube in just seconds, faster than the accompanying peristaltic waves. When the bolus or liquid reaches the lower esophageal sphincter, it presses against the sphincter, causing it to open. The material then passes into the stomach.
Digestive activities in the stomach
Gastric juices begin to flood the stomach even before food arrives. The sight, smell, taste, or even thought of food triggers the central nervous system to send nerve impulses to the gastric glands, which respond by secreting gastric juice. Once food does arrive in the stomach and touches its lining, cells in the lining release gastrin, a hormone. Gastrin, in turn, stimulates the production of even greater amounts of gastric juice.
As food fills the stomach, its wall begin to stretch. This initiates mechanical digestion in the stomach. The muscles in the walls being to contract, compressing and pummeling the food, breaking it apart physically. At the same time, the food is being mixed with gastric juices, and chemical digestion begins. Pepsin, the protein-digesting enzyme in gastric juice, starts to break down complex proteins. Little digestion of carbohydrates or fats takes place in the stomach. Water, alcohol, and drugs such as aspirin, however, are absorbed through the walls of the stomach into the bloodstream.
Once the food has been well mixed and broken down into chyme, peristalsis begins in the lower portion of the stomach. Chyme is moved downward into the pylorus. With each contraction of the stomach walls, the pyloric sphincter opens just a little, allowing a bit of chyme to squirt into the duodenum of the small intestine. When the duodenum is filled and its wall stretched, a nerve impulse is sent to the stomach to slow down its activity. It takes about four hours for the stomach to empty completely after receiving a well-balanced meal. If that meal contains much fat, then the process could take six or more hours.
Digestive activity in the small intestine
When chyme from the stomach enters the small intestine, it contains proteins and carbohydrates that have been only partially digested. Fats have been hardly digested. Over a three-to six-hour period, as chyme moves through the twists and coils of the small intestine, chemical digestion increases. By the time chyme reaches the end of the small intestine, eighty percent of all digestion in the body has taken place.
The presence of chyme in the duodenum stimulates the secretion of intestinal juice. Cells in the lining of the duodenum are also stimulated to produce hormones that, in turn, stimulate the pancreas to produce pancreatic juice and the liver to produce bile (the gall bladder is also stimulated to release its store of concentrated bile). Both enter the duodenum and combine with intestinal juice to digest or break down proteins, carbohydrates, and fats.
Peristalsis occurs in the small intestine, mixing the chyme with the intestinal juices and moving it through the organ. Although water and nutrients are absorbed all along the length of the small intestine, most absorption occurs in the jejunum. In this section, digested carbohydrates, fats, proteins, and most of the vitamins, minerals, and iron are absorbed. These nutrients pass through the walls of the villi into the blood capillaries and lacteals (lymph capillaries). The blood capillaries eventually drain into veins that connect with the portal vein, which transports the nutrient-rich blood to the liver. The lacteals, carrying fat nutrients, eventually drain into larger lymph vessels that connect with the venous system.
By the time material enters the ileum, the last section of the small intestine, all that remains is some water, indigestible food matter (such as plant fibers), and bacteria. This material then enters the large intestine through the ileocecal valve, which closes to prevent material from flowing backward.
Digestive activities in the large intestine
The large intestine does not produce any digestive enzymes; therefore, no digestion takes place. It functions mainly to absorb water and a few minerals from the waste products of digestion. Peristalsis in the large intestine occurs very slowly: material takes between twelve and twenty-four hours to pass through.
Millions of bacteria living in the large intestine feed on the waste products. In doing so, they produce vitamin K and some B vitamins that are absorbed through the wall of the large intestine into the bloodstream and then transported to the liver. The bacteria also produce intestinal gas—methane and hydrogen sulfide—that gives feces their characteristic odor. The amount of that gas, properly known as flatus, may increase if certain foods rich in carbohydrates (such as beans) are eaten.
Anorexia nervosa (an-ah-REK-seeah ner-VO-sa): Eating disorder usually occurring in young women that is characterized by an abnormal fear of becoming obese, a persistent aversion to food, and severe weight loss.
Appendicitis (ah-pen-di-SIGH-tis): Inflammation of the appendix.
Biliary atresia (BILL-ee-a-ree ah-TREE-zee-ah): Condition in which ducts to transport bile from the liver to the duodenum fail to develop in a fetus.
Bulimia (boo-LEE-me-ah): Eating disorder characterized by eating binges followed by selfinduced vomiting or laxative abuse.
Cirrhosis (si-ROW-sis): Chronic disease of the liver in which normal liver cells are damaged and then replaced by scar tissue.
Crohn's disease (CRONES di-ZEEZ): Disorder that causes inflammation and ulceration of all the layers of the intestinal wall, particularly in the small intestine.
Diverticulosis (di-ver-ti-cue-LOW-sis): Condition in which the inner lining of the large intestine bulges out through its muscular wall; if the bulges become infected, the condition is called diverticulitis.
Gallstones (GAUL-stones): Solid crystal deposits that form in the gall bladder.
Hepatitis (hep-a-TIE-tis): Inflammation of the liver, caused mainly by a virus.
Lactose intolerance (LAK-tose in-TOL-er-ance): Inability of the body to digest significant amounts of lactose, the predominant sugar in milk.
Ulcer (digestive) (UL-sir): Any sore that develops in the lining of the lower esophagus, stomach, or duodenum.
Ulcerative colitis (UL-sir-a-tiv ko-LIE-tis): Disorder that causes inflammation and ulceration of the inner lining of the large intestine and rectum.
When powerful peristaltic contractions force the feces or compacted waste products from the sigmoid colon into the rectum, the wall of the rectum stretches. This triggers the defecation reflex. Signals from the spinal cord cause the walls of the sigmoid colon and rectum to contract and the anal sphincters to relax. Feces are then eliminated through the anus. The outer sphincter muscle can be controlled voluntarily, allowing an individual to delay defecation when necessary.

Comment about this article, ask questions, or add new information about this topic: