The Cardiovascular System - Design: parts of the cardiovascular system
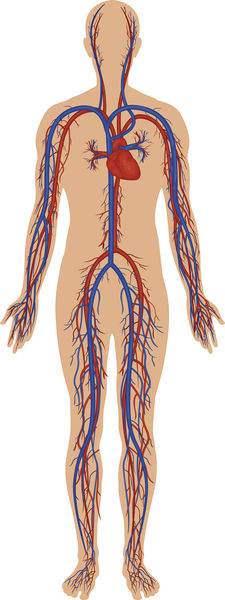
Cardiovascular comes from the Greek word cardia , meaning "heart," and the Latin vasculum , meaning "small vessel." The basic components of the cardiovascular system are the heart, the blood vessels, and the blood. The system can be compared to a large muscular pump (the heart) that sends a fluid (blood) through a series of large and small tubes (blood vessels). As blood circulates through the increasingly intricate system of vessels, it picks up oxygen from the lungs, nutrients from the small intestine, and hormones from the endocrine glands. It delivers these to the cells, picking up carbon dioxide (formed when cells use sugars or fats to produce energy) and other wastes in return. The blood then takes these waste products to the lungs and kidneys, where they are excreted.
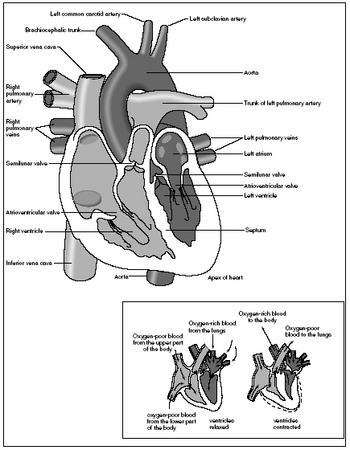
The heart
The heart is a hollow, cone-shaped muscular organ located behind and slightly to the left of the sternum or breastbone. Nestled between the lungs, the heart sits within a protective, bony cage formed by the sternum, ribs, and spine. The lower tip of the heart, called the apex, points toward the left hip and rests on the diaphragm (a membrane of muscle separating the chest cavity from the abdominal cavity). The upper portion of the heart, called the base, points toward the right shoulder and lies beneath the second rib. It is from the base that the major blood vessels of the body emerge.
The heart is about the size of a clenched fist. At birth, an infant's heart and fist are about the same size. As a human body develops, the heart and fist grow at about the same rate. In adults, an average heart weighs between 9 and 11 ounces (255 and 310 grams). It is slightly larger in males than in females.
- Agglutination (ah-glue-ti-NA-shun):
- Clumping of blood cells brought about by the mixing of blood types.
- Alveoli (al-VEE-oh-lie):
- Air sacs of the lungs.
- Antibody (AN-ti-bod-ee):
- Specialized substance produced by the body that can provide immunity against a specific antigen.
- Antigen (AN-ti-jen):
- Any substance that, when introduced to the body, is recognized as foreign and activates an immune response.
- Aorta (ay-OR-ta):
- Main artery of the body.
- Arteriole (ar-TEER-e-ohl):
- Small artery.
- Artery (AR-te-ree):
- Vessel that carries blood away from the heart.
- Atria (AY-tree-a):
- Upper chambers of the heart that receive blood from the veins.
- Atrioventricular (AV) node (a-tree-oh-ven-TRICK-ular):
- Node of specialized tissue lying near the bottom of the right atrium that fires an electrical impulse across the ventricles, causing them to contract.
- Atrioventricular (AV) valves:
- Valves located between the atria and ventricles.
- Blood pressure:
- Pressure or force the blood exerts against the inner walls of the blood vessels.
- Capillary (CAP-i-lair-ee):
- Minute blood vessel that connects arterioles with venules.
- Cardiac cycle (CAR-dee-ack):
- Series of events that occur in the heart during one complete heartbeat.
- Cholesterol (ko-LESS-ter-ol):
- Fatlike substance produced by the liver that is an essential part of cell membranes and body chemicals; when present in excess in the body, it can accumulate on the inside walls of arteries and block blood flow.
- Diaphragm (DIE-ah-fram):
- Membrane of muscle separating the chest cavity from the abdominal cavity.
- Diastole (die-ASS-te-lee):
- Period of relaxation and expansion of the heart when its chambers fill with blood.
- Diffusion (dif-FEW-shun):
- Movement of molecules from an area of greater concentration to an area of lesser concentration.
- Endocardium (en-doe-CAR-dee-um):
- Thin membrane lining the interior of the heart.
- Epicardium (ep-i-CAR-dee-um):
- Lubricating outer layer of the heart wall and part of the pericardium.
- Erythrocyte (e-RITH-re-site):
- Red blood cell.
- Filtration (fill-TRAY-shun):
- Movement of water and dissolved materials through a membrane from an area of higher pressure to an area of lower pressure.
- Hemoglobin (HEE-muh-glow-bin):
- Iron-containing protein pigment in red blood cells that can combine with oxygen and carbon dioxide.
- Hepatic portal circulation (heh-PAT-ick POR-tal):
- System of blood vessels that transports blood from the digestive organs and the spleen through the liver before returning it to the heart.
- Interstitial fluid (in-ter-STI-shul):
- Fluid found in the spaces between cells.
- Leukocyte (LUKE-oh-site):
- White blood cell.
- Megakaryocyte (meg-ah-CARE-ee-oh-site):
- Large cell in the red bone marrow that breaks up into small fragments that become platelets.
- Myocardium (my-oh-CAR-dee-um):
- Cardiac muscle layer of the heart wall.
- Osmosis (oz-MOE-sis):
- Diffusion of water through a semipermeable membrane.
- Pericardium (pair-i-CAR-dee-um):
- Tough, fibrous, two-layered membrane sac that surrounds, protects, and anchors the heart.
- Plasma (PLAZ-muh):
- Fluid portion of blood.
- Platelets (PLATE-lets):
- Irregular cell fragments in blood that are involved in the process of blood clotting.
- Pulmonary circulation (PULL-mo-nair-ee):
- System of blood vessels that transports blood between the heart and lungs.
- Purkinje fibers (purr-KIN-gee):
- Specialized cardiac muscle fibers that conduct nerve impulses through the heart.
- Red blood cells:
- Most numerous blood cells in the blood, they carry oxygen bonded to the hemoglobin within them.
- Semilunar valves (sem-eye-LOO-nar):
- Valves located between the ventricles and the major arteries into which they pump blood.
- Serous fluid (SIR-us):
- Clear, watery, lubricating fluid produced by serous membranes, which line body cavities and cover internal organs.
- Sinoatrial (SA) node (sigh-no-A-tree-al):
- Node of specialized tissue lying in the upper area of the right atrium that fires an electrical impulse across the atria, causing them to contract.
- Sinusoids (SIGH-nuh-soids):
- Larger than normal capillaries whose walls are also more permeable, allowing proteins and blood cells to enter or leave easily.
- Sphygmomanometer (sfig-moe-ma-NOM-i-tur):
- Instrument used to measure blood pressure.
- Systemic circulation (sis-TEM-ick):
- System of blood vessels that transports blood between the heart and all parts of the body other than the lungs.
- Systole (SIS-te-lee):
- Rhythmic contraction of the heart.
- Thrombocyte (THROM-bow-site):
- Platelet.
- Vein (VAIN):
- Vessel that carries blood to the heart.
- Vena cava (VEE-na KAY-va):
- Either of two large veins that return blood to the right atrium of the heart.
- Ventricles (VEN-tri-kuls):
- Lower chambers of the heart that contract to pump blood into the arteries.
- Venule (VEN-yool):
- Small vein.
- White blood cells:
- Cells in blood that defend the body against viruses, bacteria, and other invading microorganisms.
The pericardium is a tough, fibrous membrane sac that surrounds, protects, and anchors the heart. It is composed of three layers. The thin inner layer tightly hugs the outer surface of the heart and is actually a part of the heart wall. The fibrous outer layer protects the heart and anchors it to surrounding structures such as the sternum and diaphragm. The inner portion of this outer layer is lined by another layer, which produces serous fluid. This watery lubricant between the inner and outer layers of the pericardium allows the layers to slide smoothly across each other, reducing friction when the heart beats.
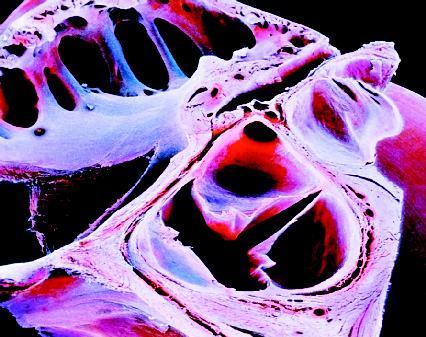
The heart wall is made up of three layers: the epicardium, the myocardium, and the endocardium. The outer layer, the epicardium, is actually the thin inner layer of the pericardium. The middle layer, the myocardium, is a thick layer of cardiac muscle that contracts to force blood out of the heart. The inner layer, the endocardium, is a thin, glistening membrane that allows blood to flow smoothly through the chambers of the heart.
HEART CHAMBERS. The heart is divided into four chambers. A muscular septum or partition divides it into a left and right side. Each side is further divided into an upper and lower chamber. The upper chambers, the atria (singular atrium), are thin-walled. They are the receiving chambers of the heart. Blood flows into them from the body, which they then pump to the ventricles, the lower heart chambers. The ventricles are the discharging chambers of the heart. Their walls are thicker and contain more cardiac muscle than the walls of the atria. This enables the ventricles to contract and pump blood out of the heart to the lungs and the rest of the body.
As blood flows from one chamber to the next, one-way valves prevent the blood from flowing backward. The valves located between the atria and ventricles are called atrioventricular or AV valves. The left AV valve (between the left ventricle and left atrium) is the mitral or bicuspid valve. The right AV valve (between the right atrium and right ventricle) is the tricuspid valve. The valves located between the ventricles and the major arteries into which they pump blood are called semilunar valves. The pulmonary semilunar valve is located between the right ventricle and the pulmonary trunk. The aortic semilunar valve is located between the left ventricle and the aorta.
The valves open and close in response to pressure changes in the heart. Each set operates at a different time. The AV valves are open when the heart is relaxed and closed when the ventricles contract. The semilunar valves are closed when the heart is relaxed and forced open when the ventricles contract. The closing of the heart valves generates the "lub-dup" sounds that a physician hears through a stethoscope. The AV valves produce the "lub" sound; the semilunar valves produce the "dup" sound.
The heart is equipped with its own nervous system that controls its beating activity. This system, called the intrinsic conduction system, is located within the heart tissue. Nerve impulses sent out through the system cause parts of the heart to contract at various times. A small node of specialized muscle tissue located in the upper area of the right atrium is called the sinoatrial or SA node. Because it initiates the impulse, the SA node is known as the pacemaker. The system includes another node, the atrioventricular or AV node, located near the bottom of the right atrium just above the ventricles. The atrioventricular or AV bundle (also known as the bundle of His) is located in the upper portion of the septum between the ventricles. Two main branches leading from this bundle (called bundle branches) divide further into small fibers that spread out within the cardiac muscle of the ventricle walls. These are known as Purkinje fibers.
Blood vessels
The blood vessels form a closed transport system of tubes measuring about 60,000 miles (96,500 kilometers) in length—more than twice the distance
around the equator of Earth. The entire blood vessel system can be thought of as a series of connected roads and highways. Blood leaves the heart through large vessels (highways) that travel forth into the body. At various points, these large vessels divide to become smaller vessels (secondary roads). In turn, these vessels continue to divide into smaller and smaller vessels (one-lane roads). On its return trip, the blood travels through increasingly larger and larger vessels (one-lane roads merging into secondary roads merging into highways) before eventually reaching the heart.
Up until only about 350 years ago, people believed blood in the body flowed back and forth like ocean tides. The ancient Greeks were the first to put forth this theory. They believed blood moved away from the heart, then ebbed back to it carrying impurities in the same vessels. This theory remained unchallenged for 1,400 years.
In 1628, English physician William Harvey (1578–1657) published a new concept of blood circulation. He maintained that there was a constant flow of blood through the arteries that returned to the heart through the veins. This formed a continuing circular flow of blood through the body.
Harvey's theory was immediately scorned, as it contradicted the basis of medical knowledge at the time. Some thirty years later, however, his idea was validated by the discovery of capillaries. Because of his pioneering work, Harvey is considered by many to be the father of modern medicine.
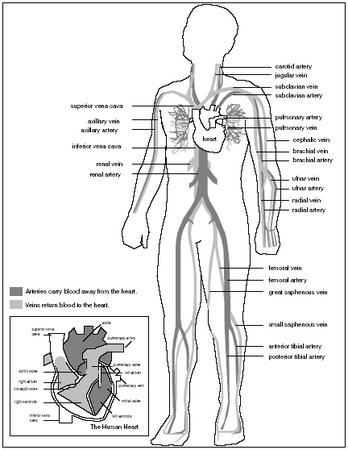
Arteries, capillaries, and veins are the main parts of this transport system. Arteries are the vessels that carry blood away from the heart. Large arteries leave the heart and then branch into smaller ones that reach out to various parts of the body. These divide even further into smaller vessels called arterioles. Within the tissues, arterioles divide into microscopic vessels called capillaries. The exchange of materials between the blood and the cells occurs through the walls of the capillaries. Before leaving the tissues, capillaries merge to form venules, which are small veins. As these vessels move closer to the heart, they merge to form larger and larger veins.
The main blood vessels differ in their structure. Although the walls of both arteries and veins are composed of three coats, they vary in thickness. Arteries have thicker inner and middle coats, which makes them more elastic. They can expand and contract easily when blood pumped from the heart surges through them. Veins, on the other hand, have thinner walls. This allows skeletal muscles surrounding them to contract and press against their flexible walls, squeezing the blood along as it returns to the heart. One-way valves in the walls of veins prevent backflow, keeping the blood flowing in one direction. The valves are most numerous in the legs, where blood must flow against the force of gravity on its way back to the heart. Unlike arteries or veins, the walls of capillaries are only one cell thick. In most capillaries, these singular cells are not joined together tightly. Because of this, oxygen, nutrients, and wastes are able to pass easily between the blood and the surrounding interstitial fluid, which fills the spaces between cells.
THE PULMONARY AND SYSTEMIC CIRCULATIONS. There are two main circulation circuits or routes in the body: the pulmonary circulation and the systemic circulation. Vessels involved in the pulmonary circulation transport blood between the heart and the lungs. Vessels in the systemic circulation transport blood to all other body parts.
The main artery of the systemic circulation is the aorta. In adults, the aorta is about the same size as a standard garden hose. It emerges upward out of the left ventricle for about an inch, then curves left over the heart (a portion called the aortic arch) before plunging downward to divide into branches that carry blood to the major parts of the body.
Branches of the aorta include the carotid arteries (which carry blood to the head), coronary arteries (which supply blood to the muscles of the heart), brachial arteries (which carry blood down the arms), and femoral arteries (which carry blood down the thighs).
The vena cava is the largest vein of the systemic circulation. It has two branches: the superior vena cava accepts blood drained from the head and arms; the inferior vena cava accepts blood drained from the lower body. Both sections (collectively called the venae cavae) empty into the right atrium.
Veins that drain into the venae cavae include the jugular veins (which drain the head), brachial and cephalic veins (which drain the arms), femoral veins (which drain the thighs), and iliac veins (which drain the pelvic or hip region).
The vessels involved in the pulmonary circulation carry blood to the lungs for gas exchange (carbon dioxide is unloaded and oxygen is picked
up), then return it to the heart. The main vessels are the pulmonary arteries and the pulmonary veins. The two pulmonary arteries branch off from the pulmonary trunk, which originates from the right ventricle. The right pulmonary artery goes to the right lung, the left pulmonary artery to the left lung. After gas exchange occurs in the lungs, the oxygenated (carrying oxygen) blood is transported back to the left atrium of the heart by four pulmonary veins.
Blood
Blood is the fluid pumped by the heart through the blood vessels to all parts of the body. It is connective tissue. As its name suggests, connective tissue connects body parts, providing support, storage, and protection. Found everywhere in the body, connective tissue is the most abundant type of the four types of tissues (the other three are epithelial, muscle, and nervous). Of all the tissues in the body, blood is unique—it is the only one that is fluid.
Blood has many functions in the body. It carries everything that must be transported from one place to another within the body: oxygen and nutrients to the cells, hormones (chemical messengers) to the tissues, and waste products to organs responsible for removing them from the body. It helps protect the body by clotting and by acting as a defense against foreign microorganisms. It also keeps the body at a constant temperature by taking heat away from cells.
Stickier and heavier than water, blood ranges in color from scarlet to dull red, depending on the amount of oxygen it is carrying (the brighter the color, the greater the amount of oxygen). Inside the body, blood has a temperature of about 100.4°F (38°C). It makes up approximately 8 percent of a person's body weight. A man of average weight has about 6 quarts (5.6 liters) of blood in his body; a woman of average weight has about 4.8 quarts (4.5 liters). Men tend to have more blood than women due to the presence of testosterone, the male sex hormone that also stimulates blood formation.
Blood is composed of both solid and liquid elements. Red blood cells, white blood cells, and platelets are the solid components that are suspended in plasma, a watery, straw-colored fluid. The living blood cells make up about 45 percent of the blood; the nonliving plasma makes up the remaining 55 percent.
PLASMA. Plasma is approximately 92 percent water. Over 100 different substances are dissolved in this fluid, including nutrients, respiratory gases, hormones, plasma proteins, salts, and various wastes. Of these dissolved substances, plasma proteins are the most abundant. These proteins, most of which are produced by the liver, serve a variety of functions. Fibrinogen is an important protein that aids in blood clotting. Albumins help to keep water in the bloodstream. Proteins called gamma globulins act as antibodies, which are substances produced by the body to help protect it against foreign substances.
The salts present in plasma include sodium, potassium, calcium, magnesium, chloride, and bicarbonate. They are involved in many important body functions, including muscle contraction, the transmission of nerve impulses, and the regulation of the body's pH (acid-base) balance.
RED BLOOD CELLS. Red blood cells, or erythrocytes, are the most prevalent of the three types of blood cells. They number about five million per cubic millimeter of blood (a cubic millimeter is an extremely small drop that is barely visible). Their main function is to transport oxygen from the lungs to all cells in the body. Red blood cells are tiny, flattened, disk-shaped structures with depressed centers: under a microscope they look like small doughnuts. Their size allows them to squeeze through the microscopic capillaries.

The four main blood types—A, B, O, and AB—were discovered by medical researchers in the early twentieth century. This discovery greatly improved the effectiveness of blood transfusions. At the time, however, whole blood could only be kept for seven days before it perished. The problem of having the appropriate blood type readily available during emergencies still existed.
In the late 1930s, American surgeon Charles Drew (1904–1950) began to explore the possibility of using plasma as a substitute for whole blood in transfusions. Because plasma lacks red blood cells, it can be given to any patient, regardless of that patient's blood type. This property makes plasma ideal for use in emergencies.
By 1940, Drew had devised a method to process and preserve blood plasma through dehydration so that it could be shipped over great distances and stored for long periods of time. When it was needed, the dried, powderlike plasma was then reconstituted or reformed through the addition of water.
The use of plasma for transfusions proved especially useful during World War II (1939–45), when there was a desperate shortage of blood to treat the wounded. Because of his research, Drew is credited with saving countless numbers of lives.
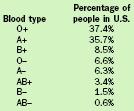
| Blood type | Percentage of people in U.S. |
| O+ | 37.4% |
| A+ | 35.7% |
| B+ | 8.5% |
| O− | 6.6% |
| A− | 6.3% |
| AB+ | 3.4% |
| B− | 1.5% |
| AB− | 0.6% |
In adults, red blood cells are formed in the red bone marrow of the ribs, vertebrae, sternum, and pelvis (marrow is the spongylike material that fills the cavities inside most bones). The primary element of red blood cells is a protein pigment called hemoglobin. Hemoglobin molecules account for one-third the weight of each red blood cell. At the center of each hemoglobin molecule is a single atom of iron, which gives red blood cells their color. In the lungs, the iron atoms combine with oxygen to create compounds called oxyhemoglobins. The main function of red blood cells is to transport this form of oxygen to the cells throughout the body. After the oxygen is transferred, hemoglobin combines with the carbon dioxide given off by the cells, and the red

blood cells carry it back to the lungs, where some of the carbon dioxide is exhaled.
Because red blood cells are constantly squeezing through tiny capillaries, their membranes receive much wear and tear. For this reason, each red blood cell lives only about four months. New red blood cells are constantly being produced in the bone marrow to replace old ones.
BLOOD TYPES. On their membranes, red blood cells carry proteins called antigens, or substances that the body recognizes as foreign. These inherited antigens determine to what blood group a person belongs: A, B, AB, or O. A person whose red blood cells carry the A antigen is type A. A person with the B antigen is type B. A person with both A and B antigens is type AB. A person with no antigens is type O.
Knowing a person's blood type is important for blood transfusions. A person with type A blood cannot receive type B blood because they carry antibodies to B antigens. B types carry antibodies to A antigens. AB types do not carry any antibodies to antigens, but O types carry antibodies to both A and B antigens. If a person is given the wrong type of blood, the blood cells clump together and can block small blood vessels. This reaction, called agglutination, can be fatal.
Another type of antigen carried on red blood cells is called the Rh antigen (so named because it was originally identified in Rh esus monkeys). Most Americans are Rh positive (Rh+), meaning they carry the Rh antigen. Rh negative (Rh−) people do not. Unlike the ABO blood group system, antibodies to the Rh antigen are not automatically found in the blood. The only problem that may arise with the Rh antigen and blood transfusions is when an Rh− individual is given Rh+ blood. In response, that person's body develops antibodies to the Rh+ antigen. Any further transfusions with Rh+ blood would then result in the previously formed antibodies attacking the donor blood.
WHITE BLOOD CELLS. White blood cells, or leukocytes, are far less numerous than red blood cells. Numbering between 4,000 and 11,000 per cubic millimeter of blood, they account for less than 1 percent of total blood volume. Despite their low numbers, white blood cells have a specialized function, serving as an important part of the body's immune system. They help defend the body against damage by bacteria, viruses, parasites, and tumor cells. Like red blood cells, white blood cells are formed in the red bone marrow (some white blood cells are produced in the lymphatic tissue as well). But whereas red blood cells are confined to the blood stream, white blood cells are not. They are able to squeeze through capillary walls on their way to an infected or damaged area of the body.
Rh factor is a special consideration during one type of pregnancy: when an Rh− woman carries an Rh+ baby. During delivery, a tear in the mother's placenta may allow a mother to be exposed to her baby's Rh+ red blood cells. (The placenta is a membrane lining the uterus through which nutrients and oxygen pass from mother to baby.) If this occurs, she then develops antibodies to the Rh+ antigen. During any subsequent pregnancy, if the woman is carrying another Rh+ baby, her anti-Rh antibodies may cross over into the baby's blood and destroy its red blood cells.
To prevent any of this from taking place, doctors will give the Rh− woman RhoGAM, an anti-Rh antibody, within seventy-two hours of her initial delivery. RhoGAM will destroy the Rh+ red blood cells that have entered her circulation before her immune system has had time to develop antibodies.
There are five kinds of white blood cells in the blood: neutrophils, eosinophils, basophils, monocytes, and lymphocytes. Each of the five plays a specific role in the body's defense system, being called into action to fight specific diseases. For example, during chronic (long-term) infections such as tuberculosis (an infectious disease of the lungs), monocytes increase in number. During asthma and allergy attacks, eosinophils increase in number.
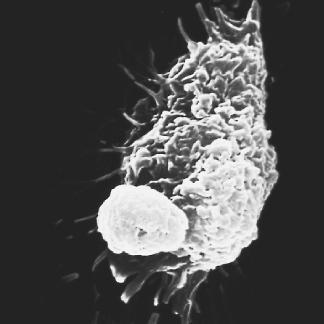
White blood cells "know" where to go in the body by following certain chemicals. When tissue is infected or damaged, it releases chemicals into the surrounding area that "attract" the proper white blood cells to fight the infection or damage. This process is known as chemotaxis.
PLATELETS. Platelets, or thrombocytes, are not truly cells like red and white blood cells. They are small, disk-shaped fragments of extraordinarily large cells called megakaryocytes that are located in bone marrow. The megakaryocytes rupture, releasing fifty or more fragments that quickly form membranes to become platelets. Numbering about 300,000 per cubic millimeter of blood, platelets help to control bleeding in a complex process called homeostasis, or the stoppage of blood flow.
When an injury to a blood vessel causes bleeding, platelets begin the clotting process by sticking to the ruptured blood vessel. As they do so, they release chemicals that attract other platelets. Soon, a clump of platelets forms a temporary plug. After this, the platelets release serotonin (sir-o-TOE-nin), a chemical that causes the blood vessel to spasm and narrow, decreasing the amount of blood flowing to the site of the injury. While this is occurring, the injured tissue releases a substance that combines with calcium and other clotting factors in blood plasma to create prothrombin activator. This activator converts prothrombin (a substance produced by the liver that is present in plasma), to thrombin (an enzyme). Thrombin then joins with fibrinogen to create long, threadlike molecules called fibrin. Fibrin molecules establish a mesh that traps red blood cells and platelets, forming the basis for the clot.

Comment about this article, ask questions, or add new information about this topic: