Autoimmune Diseases - Diabetes mellitus (dm)
Diabetes has been known for several thousand years. Late in the nineteenth century, when diabetes was well recognized as an abnormality in carbohydrate metabolism (the ability to burn sugar), several scientists discovered that the experimental removal of certain cells, the islets of Langerhans, from the pancreas, produced diabetes in dogs. This observation led to the 1921 discovery and isolation of naturally produced insulin. Insulin is a hormone produced by the islets of Langerhans. Injection of insulin into the bodies of people with diabetes proved to be the first and, to this day, the most effective means of treating the disease.
Until injectable insulin was developed, death occurred within a year or two of the onset of the disease, and usually within weeks or months of development of the symptoms. With injectable insulin, the life expectancy rose dramatically.
An early pioneer in the treatment of diabetes with insulin was Dr. Elliott Joslin of Boston. Dr. Joslin realized that the diabetic patient needed to have a full understanding of his disease so that he could take care of himself. He knew that the diabetic, with the chronic abnormality of a delicate and dynamic metabolic process, could not be cared for successfully solely by knowledgeable physicians. The patient and his family had to be informed about the disease and be active in the day-to-day management of diabetes.
In many ways this marked the beginning of what has become patient-management of illness. It is important for every type of illness and injury, but it is essential to the welfare of patients with chronic illness.
Characteristics of Diabetes
The fundamental problem in diabetes is the body's inability to metabolize glucose (burn sugar), fully and continually. This is a vital process in creating body cell energy. Glucose is a chemical derivative of carbohydrates in food after they have been digested. Carbohydrates are mostly from plants. They may come in the form of starches (such as corn), sucrose (regular sugar), and fructose (fruit sugars). All natural sweeteners, including honey, are forms of sugar. Nonnatural sweeteners such as Equal, Sweet and Low, and others are not sugar and do not affect the body the same way.
Glucose is stored under normal conditions in the form of glycogen, an animal starch, in the liver and muscles for use later as energy fuel. It is reconverted to glucose and burned by the body when energy is needed.
Insulin
Insulin is necessary for both the storage and reconversion of glucose. The metabolic failure to burn sugar may occur because of an insufficiency of insulin, an inability of the body to respond to the normal triggers for producing insulin, or for a combination of those reasons. In any event, the failure to metabolize glucose results in an abnormal, and unhealthy, accumulation of sugar in the bloodstream.
This failure to break down sugar resembles starvation in its effect. A starved person eats no food, and the diabetic eats food but is unable to gain the benefits of the food because the body is unable to break the food down into a usable form. Eventually the body will start to digest fat, protein, and muscle cells from the body to maintain the energy level. This causes a rise in acid level in the blood which, when left untreated, will cause coma and death. Before insulin was discovered, this was why diabetics died.
For most of the 20th century, insulin was prepared commercially in the United States from beef or pork pancreas. There were difficulties from this because of allergic reactions in some patients. Patients who required insulin injections but were allergic to it also had to use steroids and other immune suppressing substances to keep the allergic reaction down. This made them more susceptible to other infections.
Researchers developed an insulin drug that is manufactured with an synthetic duplicate of human genes. Unlike animal insulins, Humulin, the first consumer health product made with DNA, can be produced in unlimited quantities. It has far fewer side effects and is less costly to produce. Research continues to refine and improve the quality of injectable insulin. The effort is to get insulin to match the body's natural insulin as closely as possible in both genetic structure and the speed with which it interacts with sugar.
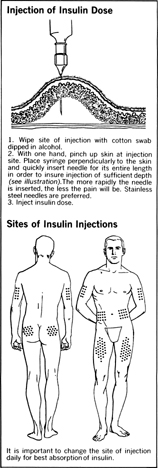
Insulin is given by injection, usually subcutaneously (under the skin), because the stomach acids will destroy it, if it is swallowed. Insulin comes in several versions, classified by the speed with which it works. Fast-acting insulin usually follows a mealtime schedule. Slow-acting insulin is for evening, and periods between meals. A combination may be administered.
How insulin doses are determined
A diabetic's basic insulin dose initially has to be established by the physician, according to several factors. The severity of the disease, the general level of exercise, the general quantity of food eaten, and the general health of the patient all play a role in determining insulin needs. This is part of the reason for hospitalizing a patient after he or she is diagnosed with diabetes.
Once the dose has been established, the quantity of insulin has to be assessed before every injection. This is done through blood testing and an analysis of the expected activity level to follow the injection and the expected food consumption. The diabetic undergoes training for all these evaluations during his or her hospital stay.
Blood testing
The methods of testing blood have become much more easy and accurate in the past 10 years. A simple pinprick to a finger for a small drop of blood is all that is needed to get an accurate blood reading. Electronic monitors are available that read the blood sample automatically. If a patient cannot afford an electronic sampler, financial assistance may be available through the American Diabetics Association. After a five-year study, it was determined that the most effective method of testing and determining insulin levels in diabetics was to test blood three to four times daily. At least once a week the diabetic should waken in the middle of the night to test blood levels. With this close monitoring of the blood sugar levels, peaks in sugar or insulin levels are less extreme, and the diabetic can avoid some of the deterioration that high sugar levels can cause.

Comment about this article, ask questions, or add new information about this topic: